Running a FACISî background check requires systematic verification of healthcare professionals against the FDA Advisory Committees and Consultant Database (FACIS), a federal exclusion list. This list identifies individuals barred from participating in federal healthcare programs. Healthcare organizations must integrate FACIS screening into comprehensive background check workflows to avoid compliance violations, financial penalties, and potential harm to patient safety. However, manual screening processes introduce substantial operational delays and human error risks that can compromise hiring timelines and regulatory obligations.
Key Takeaways
- FACISî background checks verify whether healthcare job candidates appear on federal exclusion lists that ban their participation in Medicare, Medicaid, and other federal healthcare programsâÂÂmaking these screenings legally required for healthcare employers.
- Healthcare HR teams must conduct FACISî screenings before employment begins. They must also implement ongoing monthly monitoring to maintain continuous compliance with federal regulations throughout the employment lifecycle.
- Manual FACISî database searches require navigating multiple government websites and cross-referencing candidate information across inconsistent data formats. HR staff must document each verification stepâÂÂa process that typically takes 15-30 minutes per candidate when done correctly.
- Poorly conducted FACISî screenings expose healthcare organizations to Civil Monetary Penalties ranging from $10,000 to $50,000 per excluded individual employed. Organizations also risk exclusion from federal healthcare program participation.
- The FACISî screening process must work with multiple additional exclusion databases. These include the OIG LEIE, SAM.gov, and state Medicaid exclusion lists to achieve full compliance coverage.
- Healthcare organizations operating in multiple states face added complexity. Each jurisdiction maintains separate exclusion lists with varying update frequencies and data structures that require independent verification.
- Common operational bottlenecks in manual FACISî screening include database downtime during verification windows and staff turnover disrupting institutional knowledge of proper screening protocols. Inconsistent documentation practices also fail audit requirements.
- Building compliant FACISî screening workflows from scratch demands detailed written policies and staff training on database navigation. Quality control mechanisms catch verification errors. Audit trails demonstrate due diligence to regulatory agencies.
Understanding FACISî Background Checks in Healthcare Hiring
What Is a FACISî Background Check?
A FACISî background check is a specialized screening process. It verifies whether healthcare job candidates appear in the FDA Advisory Committees and Consultant Database (FACIS). This database tracks individuals who have been sanctioned, excluded, or barred from participating in federal healthcare programs. It serves as one component within a broader federal exclusion screening framework. The framework protects Medicare, Medicaid, and other government-funded healthcare programs from fraudulent practitioners and compromised professionals.
The database identifies healthcare professionals excluded from federal healthcare program participation. Exclusions result from fraud convictions, patient abuse, controlled substance violations, license revocations, or other integrity-related offenses. When a healthcare organization employs an individual listed in FACIS without proper screening, that organization becomes liable for regulatory penalties. Organizations may also face exclusion from federal program participation themselves.
Why Healthcare Organizations Must Conduct FACISî Screenings
Federal regulations ban healthcare organizations from employing excluded individuals in any capacity that allows them to provide billable services. These services include those billed to Medicare, Medicaid, or other federal healthcare programs. Violations trigger Civil Monetary Penalties that can reach $10,000 per item or service furnished by an excluded person. Potential penalty amounts can escalate to $50,000 per incident in cases involving aggravating factors.
Beyond immediate financial penalties, healthcare organizations that employ excluded individuals face program exclusion themselves. This outcome terminates their ability to receive Medicare and Medicaid reimbursements. For hospitals, clinics, and healthcare systems that derive substantial revenue from federal program participation, such exclusions represent existential threats. The Office of Inspector General has emphasized that healthcare employers must screen prospective employees against exclusion databases before employment begins. Employers must also conduct ongoing monitoring throughout the employment relationship.
High turnover rates in healthcare professions create scenarios where quick hiring decisions may bypass proper screening protocols. Urgent staffing needs in clinical environments add pressure to speed up timelines. A single missed FACIS verification can cascade into significant regulatory exposure. This risk increases when excluded individuals provide patient care services over extended periods before anyone detects the violation.
Building or losing trust happens before an employee ever begins their employment. Doing some due diligence in compliance screening reveals how easily slipping up can lead to big trouble for an organization. I have seen where screening was approached as no big deal, a mere task to accomplish, only to be identified as an avoidable loophole down the line.
The Regulatory Framework Behind FACISî Requirements
The Social Security Act Section 1128 establishes the foundational authority for federal healthcare program exclusions. Section 1862 specifically bans payment for services furnished by excluded individuals. These statutory provisions create strict liability standards. Healthcare organizations cannot claim ignorance of an employee's excluded status as a defense against penalties once regulators discover a violation.
| Regulatory Source | Compliance Requirement |
| Social Security Act Section 1128 | Authorizes OIG to exclude individuals from federal healthcare programs |
| Social Security Act Section 1862 | Bans federal payment for services by excluded persons |
| OIG Special Advisory Bulletin | Requires pre-employment screening and ongoing monitoring |
| CMS Guidance | Mandates verification before employment begins |
The Centers for Medicare & Medicaid Services (CMS) and the Office of Inspector General issue additional guidance. This guidance clarifies employer screening obligations. OIG's Special Advisory Bulletin on the Effect of Exclusion states that healthcare employers must check exclusion databases before hiring employees and contractors. State-level regulations add more compliance layers that healthcare organizations must address alongside federal requirements.
The Manual FACISî Background Check Process
Locating and Accessing the FACISî Database
Healthcare HR professionals beginning the FACIS screening process must first navigate to the correct government database portal. The U.S. Department of Health and Human Services maintains the authentic FACIS database. Users can access it through official government websites. Healthcare organizations should establish written procedures that include verified URL addresses for exclusion databases. This prevents staff from accessing unofficial or outdated information sources.
Government database websites often experience maintenance windows, temporary outages, and performance slowdowns during peak usage periods. These issues can disrupt hiring workflows when verifications are needed urgently. Healthcare HR teams must build buffer time into their hiring timelines to accommodate these technical limitations.
Conducting Individual Name-Based FACISî Searches
Manual FACIS searches require entry of the candidate's full legal name. HR staff obtain this during the application process. Search effectiveness depends heavily on the accuracy and completeness of the name information provided. Healthcare organizations must establish protocols requiring candidates to disclose all names under which they have been licensed or practiced professionally. Exclusion records may be indexed under names the individual no longer uses currently.
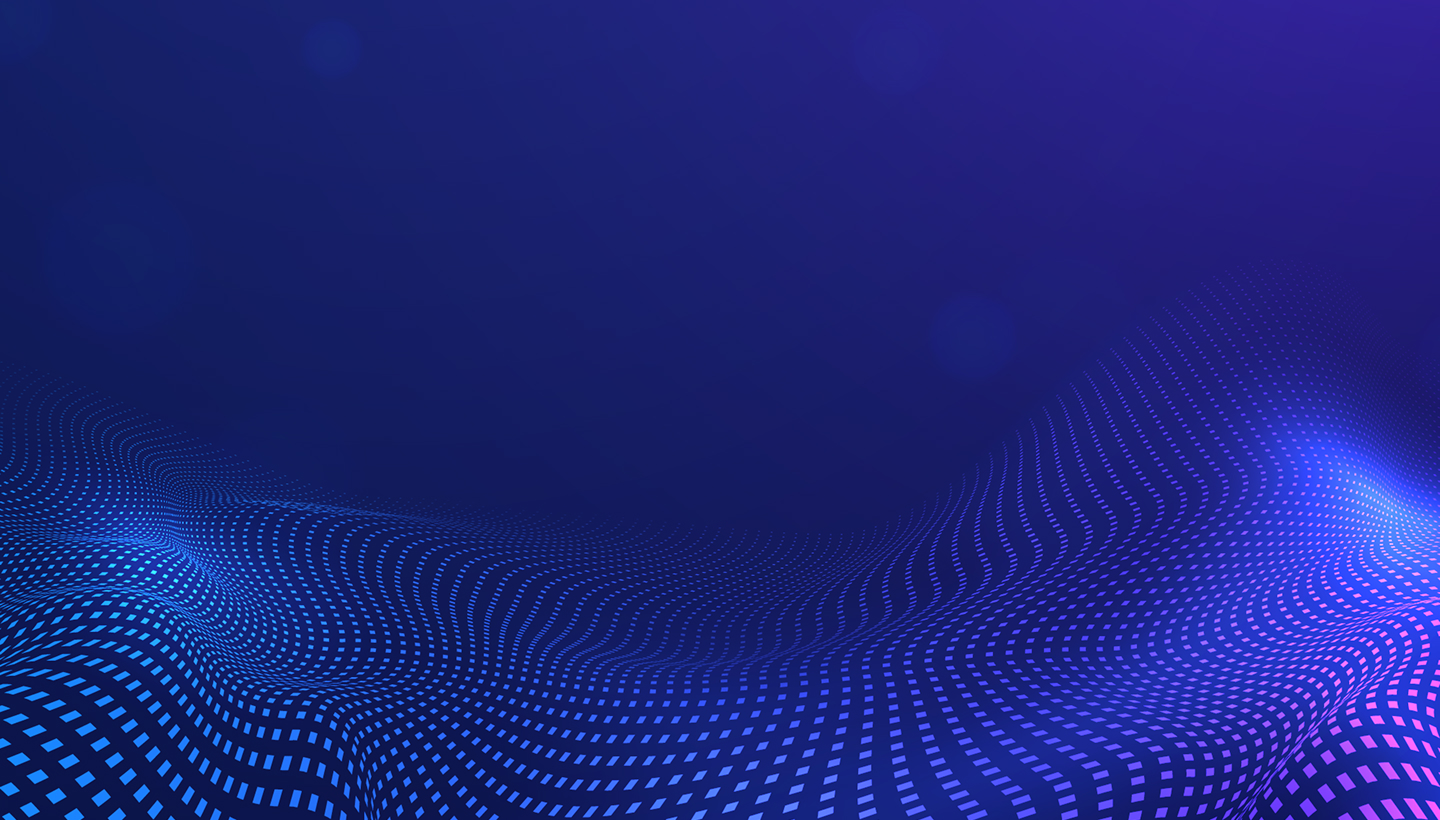
Common search execution errors include:
- Typing mistakes: Transposed letters or misspelled names during data entry cause the system to miss valid exclusion matches.
- Incomplete name variations: Omitting middle initials, prefixes, or suffixes leads to search gaps that fail to identify excluded individuals.
- Format inconsistencies: Inconsistent handling of hyphenated surnames or compound names produces unreliable search results.
- Common name confusion: Multiple similar matches require careful review using additional identifying information.
Healthcare HR coordinators rushing through high-volume screening may make mistakes. These error risks multiply when organizations lack standardized data entry protocols. Risks also increase when screening responsibilities are distributed across multiple staff members without consistent training.
Documenting and Interpreting FACISî Search Results
After completing the database search, healthcare HR professionals must properly document their findings. Documentation must satisfy regulatory audit requirements. Acceptable documentation practices include capturing screenshots of search results pages or printing PDF records of the search interface. HR staff can also record detailed written descriptions of the search parameters used. The documentation must clearly show that the search was conducted. It must specify the date and time of verification, identify the individual who performed the search, and preserve evidence of the search outcome.
| Documentation Element | Requirement | Audit Purpose |
| Search date and time | Must be recorded for every verification | Proves timely screening before employment |
| Searcher identification | Staff member name or ID required | Establishes accountability for accuracy |
| Search parameters | Full name and variations used | Shows thorough approach |
| Results captured | Screenshot or PDF of database output | Provides verifiable evidence of outcome |
| Disambiguation notes | Explanation when multiple matches occur | Shows proper evaluation of potential matches |
A positive match does not always mean immediate rejection. Healthcare organizations must carefully review the specific basis for the exclusion. They must check the effective dates of the exclusionary action. They must also determine whether any reinstatement or limitation periods apply.
Integrating FACISî Checks Into Full Background Screening

Coordinating FACISî With Other Federal Exclusion Lists
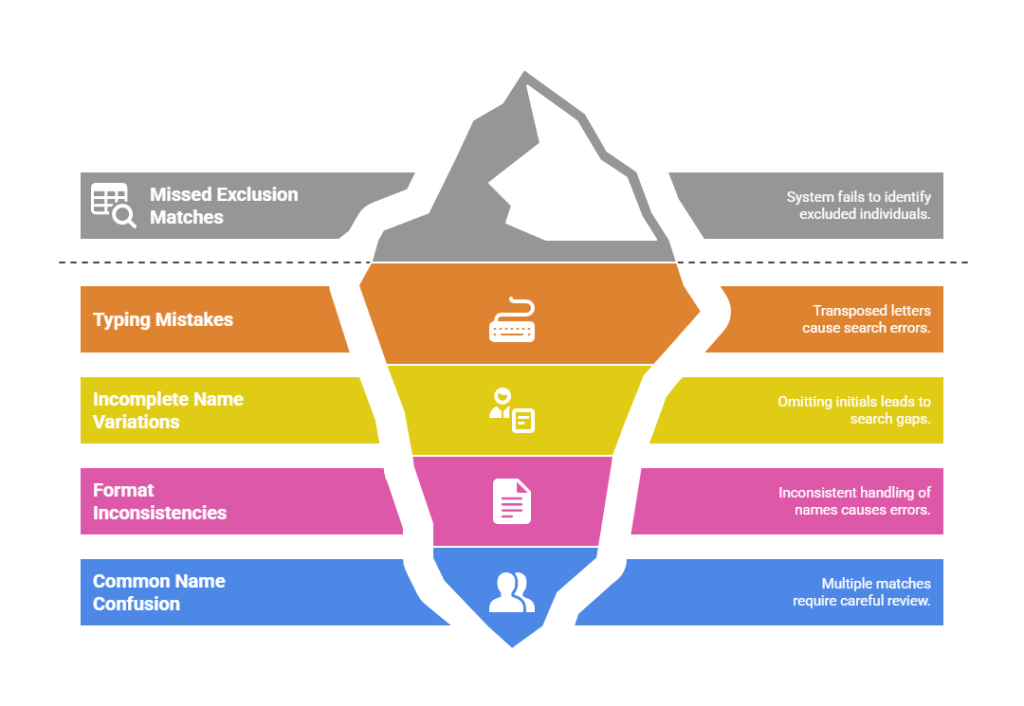
The Office of Inspector General requires employers to check the OIG List of Excluded Individuals and Entities (LEIE). This serves as the primary and most complete federal exclusion database. FACIS, SAM.gov exclusion records, and state Medicaid exclusion lists function as supplementary verification sources. These may contain exclusion information not yet reflected in the LEIE.
Required exclusion database checks include:
- OIG LEIE (List of Excluded Individuals and Entities): Primary federal exclusion database maintained by the Office of Inspector General. It contains the most complete exclusion records.
- FACIS (FDA Advisory Committees and Consultant Database): Specialized database tracking individuals sanctioned under FDA regulatory authority and healthcare program exclusions.
- SAM.gov Exclusion Records: System for Award Management database. It identifies individuals and entities barred from federal contracting and program participation.
- State Medicaid Exclusion Lists: Individual state-maintained databases. These contain providers excluded from state Medicaid programs who may not appear in federal systems.
The sequential nature of manual database checks means that a full pre-employment screening process can take 30-45 minutes per candidate when done thoroughly. Healthcare organizations hiring clinical staff for immediate placement face pressure to speed up these timelines. This creates tension between compliance thoroughness and operational urgency.
Timing FACISî Screenings Within the Hiring Lifecycle
Federal regulations require exclusion screening before the individual begins providing services. These services could generate federal healthcare program billings. Best practices recommend conducting verifications as early as feasible within the candidate evaluation process. Delaying FACIS screening until immediately before a planned start date creates significant risks. Risks increase when exclusion matches are discovered at the last moment.
The optimal timing strategy involves conducting preliminary FACIS anion screenings after extending a conditional job offer. However, organizations should complete this before finalizing employment arrangements. This approach gives healthcare organizations adequate time to investigate any potential matches. It also allows them to make final employment decisions without disrupting patient care operations.
Establishing Ongoing Monitoring and Re-Screening Protocols
The OIG recommends monthly re-screening of all employees against exclusion databases. This identifies newly added exclusions promptly. A healthcare system employing 2,000 individuals faces 24,000 individual exclusion verifications annually. This assumes proper monthly monitoring across all required databases. Manual execution of this monitoring volume requires dedicated staff time. This diverts HR resources from other essential functions.
Monthly monitoring requirements create these operational demands:

- Volume calculation: Each employee requires verification against 4-6 databases monthly. These include FACIS, LEIE, SAM.gov, and state lists. This multiplies screening workload by workforce size.
- Time allocation: Manual verification requires 5-10 minutes per employee monthly. This totals 167-333 hours monthly for a 1,000-employee organization.
- Documentation burden: Every monthly screening must be documented with date, searcher, results, and audit trail evidence. This generates thousands of records annually.
- Exception handling: Potential matches require additional investigation time beyond routine screening. This creates unpredictable workload spikes.
Healthcare organizations must preserve audit-ready evidence that each screening occurred. They must document the results and show appropriate follow-up actions.
Common Compliance Pitfalls in Manual FACISî Screening
Human Error and Data Entry Mistakes
The most common error category involves data entry mistakes during database searches. These include typing errors, transposed letters, omitted middle names, or incorrect date formats. These errors are particularly likely when HR personnel conduct high-volume screenings under time pressure. They also occur more often when staff members receive inadequate training.
Healthcare organizations face particular risk when employee turnover disrupts institutional knowledge about proper FACIS screening procedures. A departing HR coordinator who conducted exclusion screenings may have developed informal techniques for managing database quirks and disambiguation strategies. However, these techniques were never documented in written procedures. When a replacement staff member assumes screening responsibilities without this institutional knowledge, the organization's effective compliance level deteriorates.
Incomplete Database Coverage and Missed Screenings
Healthcare organizations implementing manual FACIS screening workflows often experience gaps in database coverage. Certain exclusion lists get left out. This incomplete coverage typically occurs when HR departments misunderstand the relationship between different federal exclusion databases. An HR team that consistently screens candidates against the OIG LEIE but fails to separately verify FACIS and SAM.gov creates compliance vulnerabilities. Individuals may appear in one database before their exclusion information propagates to others.
| Coverage Gap Type | How It Occurs | Compliance Impact |
| Omitted databases | HR staff checks LEIE only, skips FACIS and SAM.gov | Misses exclusions not yet in LEIE |
| Geographic expansion gaps | New state operations added without updating screening to include state lists | State-specific exclusions undetected |
| Position category exemptions | Administrative staff screening skipped based on job type | Violates full screening requirements |
| Contractor/vendor oversight | Screening limited to employees, excludes contractors | Third-party exclusions create liability |
Geographic expansion of healthcare organizations adds to database coverage challenges. A healthcare system that begins operations in a new state must identify and incorporate that state's Medicaid exclusion list into existing screening protocols.
Poor Documentation and Audit Trail Failures
The ability to produce full audit trails showing that proper screenings occurred is often as important as the screenings themselves. Healthcare organizations that conduct FACIS background checks but fail to document them properly face the same regulatory consequences as organizations that never conducted screenings. From an auditor's perspective, an undocumented screening might as well have never happened.
Common documentation failures include:
- Decentralized filing: Screening records scattered across multiple locations prevent systematic verification of full compliance.
- Incomplete records: Documentation lacking essential elements like search dates, staff identification, or result details fails audit standards.
- Retention gaps: Older screening documentation discarded before required retention periods expire eliminates proof of historical compliance.
- Informal tracking: Individual staff spreadsheets or email folders rather than centralized systems create inaccessible records during audits.
Manual documentation systems using disconnected spreadsheets cannot realistically maintain full recordkeeping at scale.
Building Effective FACISî Screening Workflows
Developing Written Policies and Procedures
Healthcare organizations must develop full written policies. These policies should clearly define screening requirements, responsibilities, timelines, and documentation standards. Effective policy documents must go beyond general statements. They should provide detailed step-by-step instructions that HR personnel can follow reliably.
Policies must list all databases that will be checked during pre-employment and ongoing monitoring screenings. They must specify exact timing requirements. This includes when screenings will occur in the hiring process and monthly calendar schedules for ongoing monitoring. Clear responsibilities must identify which positions or departments handle conducting screenings, performing quality reviews, and maintaining documentation.
Healthcare organizations must also establish written procedures for handling positive matches and unclear search results. These procedures should define escalation pathways. They should specify who has authority to make final employment decisions when potential exclusions are identified. They should also establish timelines for completing investigations.
Training HR Staff on Proper Search Techniques
Training programs must include hands-on practice with actual database interfaces. Detailed instruction on managing common complications like name variations and disambiguation of similar matches ensures accuracy. New employee training should include supervised practice screenings. Trainees conduct FACIS searches under the observation of experienced staff.
Critical training components include:
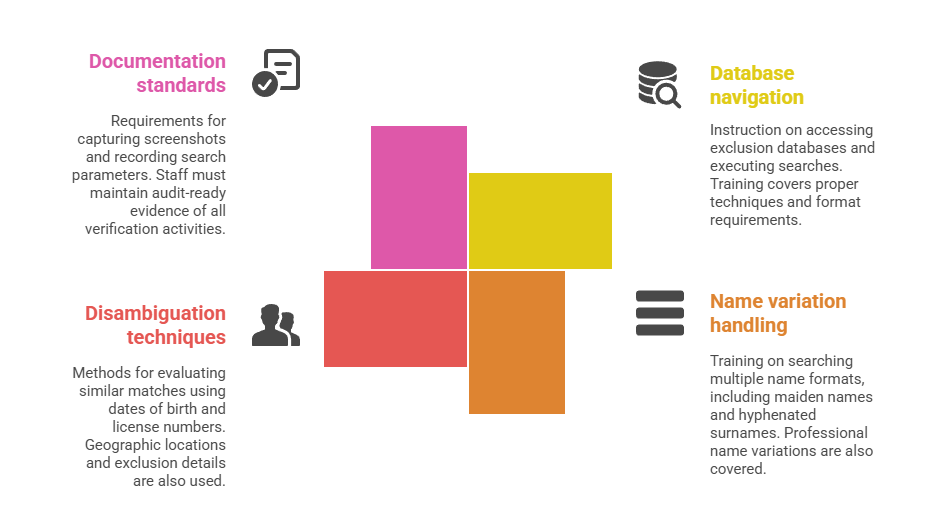
- Database navigation skills: Step-by-step instruction on accessing each required exclusion database. Training covers executing searches using proper techniques and format requirements.
- Name variation handling: Training on searching multiple name formats. These include maiden names, previous married names, hyphenated surnames, and professional name variations.
- Disambiguation techniques: Methods for evaluating multiple similar matches. Staff use dates of birth, license numbers, geographic locations, and exclusion details to identify correct individuals.
- Documentation standards: Requirements for capturing screenshots and recording search parameters. Staff must maintain audit-ready evidence of all verification activities conducted.
Periodic refresher training reinforces proper techniques. It also addresses procedural updates when database interfaces change.
Implementing Quality Control and Verification Mechanisms
Healthcare organizations must implement systematic quality control mechanisms. These catch errors and ensure consistent screening quality. Quality control programs typically involve supervisory review of a statistical sample of completed screenings. They also include periodic audits comparing screening documentation against actual hiring records.
When quality control reviews identify errors or compliance gaps, healthcare organizations must implement corrective action processes. These address both immediate issues and systemic underlying causes. If a quality review discovers that an HR coordinator consistently misspells candidate names during database searches, the immediate corrective action involves re-screening all candidates that coordinator processed. The systemic corrective action involves evaluating whether additional training, modified procedures, or verification checkpoints could prevent similar errors.
Real-World Scenarios and Compliance Consequences
Case Study: Hiring Delays From Last-Minute Exclusion Discovery
A mid-sized community hospital extended a conditional offer to an experienced emergency department physician. The hospital conducted routine FACIS and exclusion list screenings two days before the planned start date as part of final pre-employment processing. The screening revealed that the physician had been excluded from federal healthcare program participation three years earlier. The exclusion resulted from a controlled substance violation.
The hospital faced several compounding problems. The candidate had already resigned from their previous position and relocated their family to accept the hospital's offer. The emergency department was left with an unfilled physician vacancy. This created patient care capacity constraints. The hospital's recruitment process had to restart completely. This led to additional months of vacancy and recruitment costs.
This scenario shows the critical importance of conducting FACIS screenings early in the hiring process. Organizations should not defer verification until immediately before planned start dates. Had the hospital completed exclusion screenings before extending an offer, it would have identified the exclusion while alternative candidates were still available.
Case Study: Monthly Monitoring Gap Creates Extended Exposure
A regional healthcare system with 1,200 employees implemented quarterly re-screening of existing staff against exclusion databases instead of the recommended monthly frequency. During one quarter, a medical assistant working in a primary care clinic was excluded from federal healthcare program participation. The exclusion followed a fraud conviction. The healthcare system did not discover this exclusion for eleven weeks.
During those eleven weeks, the excluded medical assistant continued providing patient care services. The healthcare system billed Medicare and Medicaid for these services. When regulators finally discovered the exclusion, the healthcare system faced Civil Monetary Penalty exposure for every service the medical assistant had provided. The organization's compliance department calculated approximately 440 patient encounters during this window. Potential penalties reached millions of dollars.
Had the healthcare system implemented proper monthly monitoring, it would have detected the excluded medical assistant's status within at most four weeks rather than eleven weeks. The decision to implement quarterly monitoring based on administrative convenience created direct financial consequences. These far exceeded any staff time savings achieved.
Frequently Asked Questions
Below are the frequently asked questions regarding the process of conducting a background check. These answers cover questions asked by the employer as well as the candidate. They include what is involved, how long it will take, the rules to be followed, as well as the guidelines.
What is a FACISî background check and why is it required for healthcare employees?
A FACISî background check verifies whether healthcare job candidates appear in the FDA Advisory Committees and Consultant Database. This database identifies individuals excluded from federal healthcare programs. Federal law bans employing excluded individuals in any capacity that generates Medicare or Medicaid billings. Violations result in Civil Monetary Penalties from $10,000 to $50,000 per incident plus potential organizational exclusion.
How often do healthcare organizations need to conduct FACIS background checks?
Healthcare employers must conduct FACIS screenings before employment begins. This verifies that new hires are not excluded. Organizations must also implement ongoing monitoring that re-screens all current employees monthly against FACIS and other exclusion databases. The Office of Inspector General recommends monthly re-screening to minimize the window during which an excluded employee might provide services before detection.
What databases should be checked in addition to FACIS for full exclusion screening?
Full healthcare screening requires verification against multiple federal and state exclusion databases beyond FACIS. Organizations must check the Office of Inspector General List of Excluded Individuals and Entities (LEIE) as the primary federal exclusion database. SAM.gov exclusion records identify individuals barred from federal contracting. State Medicaid exclusion lists contain individuals excluded at state level who may not appear in federal systems.
How long does it take to conduct a manual FACIS background check?
A thorough manual FACIS screening for a single candidate typically requires 15-30 minutes when done correctly. This includes time to access the database, enter search criteria, review results, identify potential matches, and document findings. Full exclusion screening including FACIS, OIG LEIE, SAM.gov, and state databases can extend to 30-45 minutes per candidate for complete verification.
What happens if a healthcare organization employs someone who appears in the FACIS database?
Healthcare organizations employing excluded individuals face Civil Monetary Penalties reaching $10,000 per service provided by the excluded person. Penalties can escalate to $50,000 per incident in cases involving aggravating factors. Organizations also risk exclusion themselves from Medicare and Medicaid participation. This terminates their ability to receive federal reimbursements.
Can healthcare organizations conduct FACIS screenings only for clinical staff and skip administrative positions?
Federal exclusion screening requirements apply to all individuals employed by healthcare organizations. This includes individuals who do not provide direct patient care. Even administrative staff may perform functions that indirectly support services billed to federal healthcare programs. Healthcare employers cannot legally limit FACIS screenings only to clinical positions. Organizations must implement full screening covering all employees, contractors, and vendors.
What should healthcare HR staff do when FACIS search results show multiple people with similar names?
When FACIS searches return multiple individuals with similar names, HR personnel must compare additional identifying information to determine correct matches. Useful distinguishing information includes dates of birth, professional license numbers, National Provider Identifiers, and geographic locations. If staff cannot complete disambiguation with available information, organizations should request additional identifying details from the candidate before making employment decisions.
How should healthcare organizations document FACIS background checks to satisfy audit requirements?
Acceptable FACIS documentation must show that verification occurred. It must specify when the search was conducted and identify who performed the screening. Documentation must preserve evidence of results obtained. Organizations should capture screenshots or PDF records of database search result pages. They should maintain centralized tracking logs recording all screenings conducted. Organizations should implement retention systems preserving evidence for the longer of seven years or employment duration plus three years.
Can healthcare organizations use third-party vendors to conduct FACIS screenings on their behalf?
Healthcare organizations may engage qualified vendors to conduct FACIS and exclusion list screenings as part of full background check services. However, the healthcare employer retains ultimate legal responsibility for ensuring proper verifications occur. When evaluating vendors, organizations should verify that screening processes include FACIS along with all other required databases. They should confirm that verification frequency meets monthly monitoring standards.
What are the most common mistakes healthcare organizations make when conducting FACIS screenings manually?
The most common errors include typing mistakes during database searches causing missed matches. Incomplete database coverage occurs when organizations check some but not all required lists. Timing delays that allow candidates to begin work before screening completion create violations. Poor documentation fails to preserve audit-ready evidence. Implementation of quarterly or annual monitoring rather than required monthly re-screening extends exposure windows.
Additional Resources
- Office of Inspector General â List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/ - Office of Inspector General â Special Advisory Bulletin on the Effect of Exclusion from Participation in Federal Health Care Programs
https://oig.hhs.gov/exclusions/files/sab-05092013.pdf - System for Award Management (SAM) â Federal Exclusions Database
https://sam.gov/ - Centers for Medicare & Medicaid Services â Preclusion List
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/MedicareProviderSupEnroll/PreclusionList - Social Security Act Section 1128 â Exclusion of Certain Individuals and Entities
https://www.ssa.gov/OP_Home/ssact/title11/1128.htm

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.