Healthcare organizations face evolving regulatory landscapes and workforce challenges that demand robust screening infrastructure capable of adapting to 2026's compliance environment. Building resilient healthcare screening programs requires integrating federal exclusion monitoring, state-specific requirements, and operational frameworks that address hybrid workforce models while maintaining patient safety standards.
Key Takeaways
- Healthcare screening programs must function as compliance architecture, not merely administrative checkboxes, to address 2026's regulatory complexity.
- Federal exclusion monitoring through databases like the OIG List of Excluded Individuals and Entities remains a non-negotiable component of Medicare and Medicaid provider eligibility.
- State-specific healthcare screening laws create jurisdictional variance that requires systematic monitoring and adaptation mechanisms.
- Post-pandemic workforce dynamics, including staffing shortages and hybrid care models, necessitate screening protocols that balance thoroughness with operational efficiency.
- FACIS® database integration provides healthcare-specific screening capabilities that differentiate medical facility requirements from general employment verification.
- Continuous monitoring frameworks offer proactive risk management compared to point-in-time screening approaches that may miss subsequent exclusions or sanctions.
- Documentation standards and audit trails serve dual purposes as compliance evidence and operational quality indicators.
- Modern healthcare screening programs must address emerging workforce categories, including telehealth providers and contract specialists operating across state lines.
The 2026 Healthcare Screening Landscape: Regulatory Complexity and Workforce Realities
The regulatory environment governing healthcare employee screening continues to evolve as federal agencies refine enforcement priorities and state legislatures respond to workforce challenges. Healthcare organizations preparing for 2026 must recognize that screening programs function as foundational compliance architecture rather than isolated hiring procedures. Organizations should consult legal counsel regarding jurisdiction-specific compliance requirements as they develop or update screening protocols.
Federal requirements establish baseline standards, particularly regarding exclusion monitoring and provider eligibility for government healthcare programs. The Office of Inspector General maintains the List of Excluded Individuals and Entities. Healthcare employers participating in federal healthcare programs should check this list to avoid hiring individuals barred from such participation, though specific checking methodologies and frequencies are not prescribed by federal regulation and should be determined based on organizational risk assessment and legal counsel guidance. State medical boards, professional licensing authorities, and specialized databases add layers of verification requirements that vary significantly by jurisdiction and clinical role.
Compliance Architecture vs. Administrative Process
Traditional approaches often treat background screening as a one-time gate at the hiring stage. Modern compliance architecture recognizes screening as ongoing infrastructure that must adapt to regulatory changes, monitor for post-hire developments, and integrate with broader risk management systems. This shift reflects both regulatory expectations and operational realities in healthcare environments where patient safety depends on workforce integrity.
| Screening Approach | Timeline | Risk Detection | Compliance Value |
| One-time verification at hire | Single point | Pre-employment only | Minimal ongoing protection |
| Scheduled re-screening | Annual or biennial | Periodic snapshots | Delayed issue detection |
| Continuous monitoring | Real-time or daily | Immediate alerts | Proactive risk management |
Healthcare organizations operating across multiple states encounter jurisdictional complexity that generic screening approaches cannot adequately address. A registered nurse licensed in three states may face different background check requirements, lookback periods, and disqualifying offense criteria in each jurisdiction. Physicians with admitting privileges at facilities in different states must satisfy varying credentialing standards that incorporate state-specific screening elements.
Post-Pandemic Workforce Dynamics
The healthcare workforce has undergone structural changes that affect screening program design. Staffing shortages have increased reliance on travel nurses, locum tenens physicians, and contract specialists who move frequently between facilities and jurisdictions. Telehealth expansion has created clinical relationships that cross state lines, raising questions about which jurisdiction's screening standards apply when a provider in one state delivers care to patients in another.
Hybrid workforce models combine traditional employees, contracted professionals, and technology-enabled care delivery in ways that complicate screening responsibility and oversight. Healthcare organizations must determine appropriate screening standards for each workforce category while maintaining consistent patient safety protections.
In healthcare, I've learned that a background screening is never just a hiring process, but rather a component of a compliance model that is foundational to protecting our patients, our providers, and our organization. So, to HR leaders, my advice is to think about an ongoing process, not a one-time process; to think about a process that includes exclusion monitoring, licensure, and state-specific requirements, rather than just a one-time check. As our workforce model continues to evolve to incorporate telehealth and contract staff, our screening model also needs to adapt to those changes. When we build strong, well-documented processes, we're not only meeting a regulation, we're also building a culture of accountability and trust.
Healthcare-Specific Screening Components: Beyond General Employment Verification
Healthcare screening programs incorporate specialized components including federal exclusion database monitoring, professional license verification, abuse registry checks, and healthcare-specific disciplinary databases. When healthcare organizations obtain consumer reports from consumer reporting agencies as part of employment screening, they must comply with Fair Credit Reporting Act requirements, including obtaining proper authorization and following required adverse action procedures if information in a report influences an employment decision. These elements differentiate medical facility hiring from general employment processes:

- Federal exclusion database monitoring for Medicare and Medicaid participation compliance
- Professional license verification across multiple states and specialties
- Abuse registry checks at state and facility-specific levels
- Healthcare disciplinary database searches through aggregated systems
- Clinical privilege verification for hospital-based practitioners
- Controlled substance registration validation for prescribers
Understanding these components helps organizations build programs that satisfy compliance mandates while supporting operational objectives.
Federal Exclusion Monitoring and Provider Eligibility
Medicare and Medicaid participation requirements prohibit healthcare organizations from employing individuals excluded from federal healthcare programs. The OIG List of Excluded Individuals and Entities serves as the primary federal exclusion database, but comprehensive screening may also check the General Services Administration's System for Award Management, which maintains debarment records across federal programs.
Exclusions result from various causes, including healthcare fraud convictions, patient abuse, controlled substance violations, and license revocations. Exclusion periods vary, with some individuals permanently barred and others facing temporary exclusions ranging from several years to decades. Healthcare organizations that employ excluded individuals and submit claims to federal healthcare programs for services involving those individuals risk civil monetary penalties, potential exclusion of the organization itself, and loss of federal healthcare program participation. The specific consequences depend on the circumstances and applicable regulations.
FACIS® Database Integration
The Federation of State Medical Boards and similar organizations maintain databases that aggregate disciplinary actions, sanctions, and regulatory findings across state licensing boards. FACIS® database integration provides healthcare-specific screening capabilities that general criminal record checks cannot replicate.
These databases capture professional discipline that may not appear in criminal records. License suspensions, practice restrictions, malpractice settlements, and peer review findings all populate these specialized systems. A physician might have no criminal record yet face significant disciplinary history that FACIS® databases would reveal. For healthcare organizations, this information is essential to credentialing decisions and patient safety risk assessment.
State medical boards independently discipline licensees based on state-specific standards and procedures. FACIS®-type databases aggregate this dispersed information, enabling healthcare employers to identify patterns or issues across jurisdictions that individual state board checks might miss. This becomes particularly valuable for providers who have practiced in multiple states or who hold licenses in several jurisdictions.
Professional License Verification and Status Monitoring
Healthcare roles require professional licenses whose validity and status directly affect employment eligibility. License verification confirms that credentials are current, unrestricted, and appropriate for the intended clinical role. Status monitoring tracks subsequent changes, including suspensions, restrictions, or revocations that occur after initial verification.
License status changes may result from disciplinary actions, continuing education deficiencies, failure to renew, or administrative issues. Healthcare organizations must maintain systems that detect status changes promptly, particularly when those changes affect clinical practice authority or patient safety.
Professional licensing bodies increasingly offer online verification systems and notification services. However, verification requirements and available information vary by profession and state. Some licensing boards provide detailed disciplinary history and practice restrictions, while others offer only basic status confirmation.
State-Specific Healthcare Screening Laws: Jurisdictional Variance and Compliance Mapping
Healthcare organizations must navigate a complex landscape of state-specific screening requirements that vary by clinical role, practice setting, and patient population. This jurisdictional variance creates compliance challenges, particularly for multi-state healthcare systems and organizations employing professionals who practice across state lines.
Statutory Requirements and Regulatory Standards
States establish healthcare screening requirements through statutes, administrative regulations, and licensing board rules. These requirements may specify which databases must be checked, what disqualifying offenses trigger employment prohibitions, how far back screening must look, and what ongoing monitoring is necessary.
Some states mandate specific screening components for certain healthcare roles:
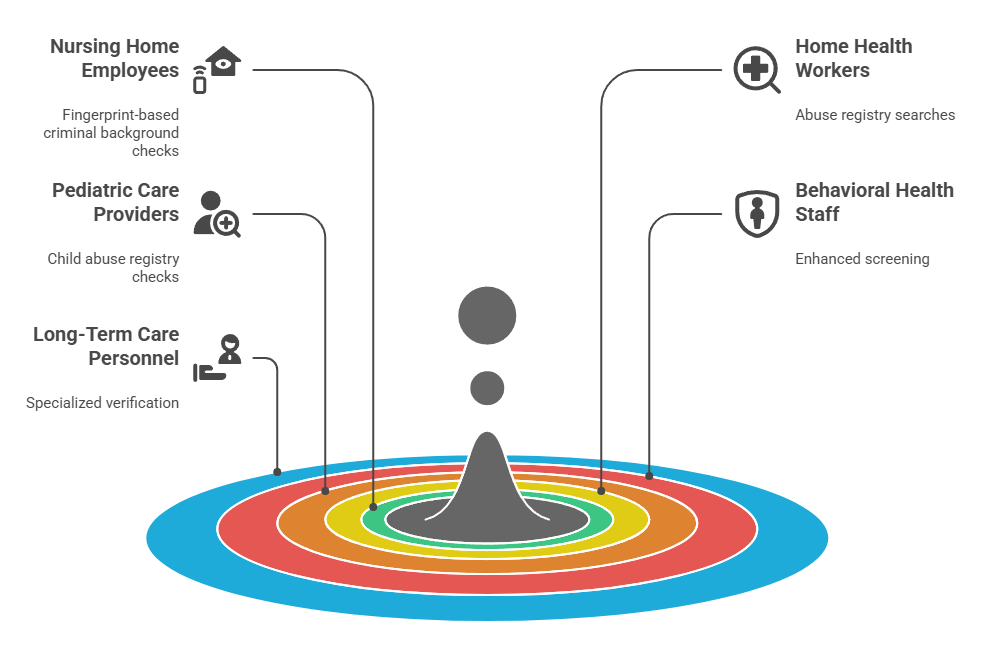
- Fingerprint-based criminal background checks for nursing home employees
- Abuse registry searches for home health workers
- Child abuse registry checks for pediatric care providers
- Enhanced screening for behavioral health facility staff
- Specialized verification for long-term care and assisted living personnel
Requirements often differ based on patient vulnerability, with more stringent standards for long-term care facilities, behavioral health settings, and facilities serving children or individuals with disabilities.
Lookback periods, which determine how far into an applicant's history screening must extend, vary by state and offense type. Some jurisdictions mandate limits on consideration of certain convictions after specified periods, prohibiting employers from considering older records. Other jurisdictions permit longer lookback periods, though organizational policies may impose additional restrictions. Employers must comply with the most restrictive applicable law in each jurisdiction.
Ban-the-Box Considerations in Healthcare
Ban-the-box laws restrict when employers may inquire about criminal history during the hiring process. These laws, which exist in numerous states and municipalities, generally prohibit criminal history questions on initial applications and may restrict when background checks can be conducted.
| Jurisdiction Type | Typical Restriction | Healthcare Exception |
| State ban-the-box laws | No inquiry until interview or conditional offer | Varies by state, often permits earlier screening for patient care roles |
| Municipal ordinances | No inquiry on application, delayed background check | Limited exemptions, depends on local law language |
| Federal contractor rules | Delayed inquiry and individualized assessment | Patient safety roles may have modified requirements |
Healthcare employers face unique considerations because patient safety obligations and regulatory requirements may create exceptions or modifications to general ban-the-box rules. Some jurisdictions exempt healthcare positions from ban-the-box restrictions, recognizing that timely criminal history screening serves patient protection purposes. Other jurisdictions apply ban-the-box rules to healthcare hiring but permit earlier screening than would be allowed in other industries.
Healthcare organizations operating in ban-the-box jurisdictions must determine which positions qualify for any available exemptions, when criminal history inquiries and checks may occur, and how to conduct individualized assessments when criminal history is identified. Individualized assessments typically require consideration of the nature and gravity of the offense, time elapsed since the offense or completion of sentence, and the nature of the job sought, consistent with applicable EEOC guidance and state or local law requirements.
Abuse Registry Requirements
Many states maintain abuse registries that document substantiated findings of abuse, neglect, or mistreatment in healthcare or caregiving settings. Healthcare employers may be required to check these registries before hiring individuals for roles involving patient care or access to vulnerable populations.
Registry requirements vary significantly by state. Some states mandate registry checks only for specific settings like nursing homes or home health agencies. Others require broader application across healthcare employment. The populations covered by registries differ, with some states maintaining separate registries for child abuse, elder abuse, and abuse of individuals with disabilities.
Interstate registry access presents practical challenges. While some states offer online registry searches, others require formal requests or provide limited access to non-governmental entities. Multi-state healthcare organizations must develop processes for checking relevant registries in each jurisdiction where they operate or where applicants have lived or worked.
Building Operational Resilience: Screening Program Infrastructure for Workforce Challenges
Effective healthcare screening programs balance regulatory compliance with operational realities, including staffing pressures, rapid hiring needs, and workforce mobility. Building operational resilience requires infrastructure that supports both thoroughness and efficiency.
Point-in-Time Screening vs. Continuous Monitoring
Traditional point-in-time screening verifies an individual's background at the hiring stage but provides no ongoing oversight. This approach creates risk exposure because exclusions, license suspensions, criminal convictions, or disciplinary actions occurring after hire remain undetected until the next scheduled re-screening, if one occurs.
Continuous monitoring frameworks check relevant databases on an ongoing basis, generating alerts when new information appears:
- Monthly or weekly exclusion database searches with automated alerts
- Real-time license status monitoring through state board integration
- Criminal record monitoring in jurisdictions where legally permitted
- Ongoing disciplinary action tracking through professional databases
Continuous monitoring offers risk management advantages by enabling prompt response to changes that affect employment eligibility or patient safety. Healthcare organizations can take corrective action immediately rather than discovering issues months or years later during re-screening.
Implementation considerations include determining which databases warrant continuous monitoring versus periodic re-screening, establishing alert response protocols, and integrating monitoring systems with human resources and compliance workflows. Not all screening components require continuous monitoring. Organizations must assess risk, regulatory requirements, and operational feasibility for each element.
Screening Protocols for Hybrid and Contingent Workforces
Healthcare staffing models increasingly incorporate travel nurses, locum tenens physicians, per diem employees, contracted specialists, and telehealth providers. Each category presents distinct screening considerations regarding responsibility, standards, and verification.
When healthcare organizations engage workers through staffing agencies, screening responsibility may be contractually allocated to the agency, the hiring organization, or shared. However, regulatory liability for employing excluded individuals or improperly credentialed providers generally remains with the healthcare organization providing patient care. Additionally, Fair Credit Reporting Act compliance obligations apply to the party that obtains consumer reports and makes or participates in employment decisions, regardless of contractual allocation of screening duties.
| Worker Category | Typical Employment Structure | Screening Responsibility | Key Verification Elements |
| Travel nurses | Agency-placed temporary staff | Shared or facility-led | License, exclusions, references, clinical competencies |
| Locum tenens physicians | Contract through placement firm | Facility maintains verification duty | Board certification, privileges, malpractice history, exclusions |
| Telehealth providers | Direct or contracted remote workers | Employer based on practice location | Multi-state licenses, exclusions, telehealth-specific regulations |
| Per diem staff | Direct hire intermittent workers | Full employer responsibility | Standard employment screening with status monitoring |
Credentialing standards for temporary or contract providers should align with standards for permanent employees in equivalent roles. Accepting a staffing agency's representation that screening has been completed without verifying the scope and recency of checks creates risk exposure.
Rapid Credentialing and Emergency Hiring Protocols
Staffing shortages and emergency situations sometimes necessitate rapid hiring processes. Healthcare organizations may implement expedited screening protocols that satisfy immediate patient care needs while maintaining safety standards.
Provisional employment arrangements permit individuals to begin work based on preliminary screening results while comprehensive checks are completed. These arrangements typically require clear results on critical safety checks, such as exclusion database searches and primary license verification, before work begins. Additional screening components, such as education verification or complete multi-state criminal record checks, may be finalized during a defined provisional period.
Provisional employment policies should specify which screening components must be complete before work begins, which may be pending, maximum provisional period duration, and supervision or practice restrictions during provisional status.
Documentation Standards, Audit Trails, and Quality Assurance
Comprehensive documentation serves multiple purposes in healthcare screening programs, providing compliance evidence, supporting quality improvement, and enabling effective audit response.
Record Retention and Accessibility
Healthcare organizations should maintain records documenting each screening component performed, results obtained, and decisions made. Regulatory requirements and accreditation standards may specify minimum retention periods, often ranging from several years to the duration of employment plus a defined period afterward.
Documentation should capture the following elements:

- Databases searched with specific identifiers and search parameters
- Dates of verification and re-verification activities
- Results obtained with copies of source documents or system screenshots
- Interpretation of findings and decision rationale
- Corrective actions taken when issues are identified
- Ongoing monitoring records with alert logs and response documentation
When screening identifies information requiring evaluation, documentation should reflect the assessment process, factors considered, and rationale for the hiring decision. This documentation becomes particularly important if decisions are later challenged or if organizations must demonstrate compliance with individualized assessment requirements under state or local laws.
Audit Trail Development
Effective audit trails enable healthcare organizations to demonstrate compliance during regulatory surveys, accreditation reviews, or legal proceedings. Audit trails should show systematic application of screening policies, timely completion of required checks, and appropriate response to identified issues.
Compliance audits may examine whether screening policies address applicable regulatory requirements, whether practices align with written policies, whether screening is completed before employment begins or within permitted timeframes, and whether ongoing monitoring occurs as required. Documentation gaps or inconsistencies identified during audits create compliance risk and may trigger expanded review.
Proactive internal auditing helps identify compliance gaps before external reviewers discover them. Regular audits of screening files, monitoring records, and credentialing documentation enable organizations to detect process failures, documentation deficiencies, or policy violations and implement corrective action.
Quality Metrics and Performance Monitoring
Healthcare organizations may track quality metrics related to screening program performance. Time from application to screening completion indicates process efficiency. Percentage of screenings completed before start date measures compliance with timing requirements. Frequency of monitoring alerts reveals system sensitivity and potential risk exposure. Rate of post-hire discoveries that screening should have detected highlights process gaps.
Performance metrics serve operational purposes by identifying bottlenecks, resource constraints, or process inefficiencies that affect hiring timelines. They also support quality improvement by highlighting areas where screening processes require strengthening or where staff need additional training.
Tracking adverse findings, such as exclusion discoveries or disqualifying criminal history, provides data for risk assessment and may inform policy decisions about screening scope or frequency. However, organizations must ensure that tracking and reporting practices comply with applicable privacy requirements, including proper handling of sensitive personal information such as Social Security numbers, dates of birth, and criminal history records, and that data retention, access controls, and reporting practices do not create unnecessary discrimination risks or violate state or federal data protection laws.
Technology, Automation, and Future Screening Methodologies
Technological capabilities continue to evolve, offering opportunities to enhance screening efficiency, accuracy, and scope. Healthcare organizations evaluating technology solutions should assess capabilities, limitations, and compliance implications.
Database Integration and Automation Tools
Technology platforms may integrate multiple data sources, automate search processes, and generate consolidated reports. Integration capabilities can reduce manual effort, decrease time to completion, and improve consistency by standardizing search processes.
Automation offers efficiency benefits but requires oversight to ensure accuracy and completeness:
- Verify database access methods and update frequency
- Understand matching algorithms and how name variations are handled
- Review processes for managing potential matches requiring manual verification
- Confirm data refresh cycles align with monitoring frequency requirements
- Test system performance periodically to detect degradation
Reliance on technology does not eliminate organizational responsibility for screening accuracy and compliance. When healthcare organizations obtain reports from consumer reporting agencies, those agencies have independent obligations under the Fair Credit Reporting Act regarding reasonable procedures to ensure maximum possible accuracy. Healthcare organizations remain responsible for using the information appropriately, following required adverse action procedures, and ensuring their screening policies comply with applicable laws.
Artificial Intelligence and Predictive Screening Approaches
Emerging technologies apply artificial intelligence or machine learning to screening processes, potentially offering capabilities such as automated record review, risk scoring, or predictive assessment. These approaches raise important questions about accuracy, fairness, transparency, and legal compliance.
| AI Application | Potential Benefit | Compliance Consideration |
| Automated record review | Faster processing of large document sets | Accuracy validation and error rate monitoring required |
| Risk scoring algorithms | Standardized assessment framework | Disparate impact testing and bias auditing necessary |
| Predictive analytics | Proactive identification of potential issues | Transparency requirements and explainability standards |
| Pattern recognition | Detection of inconsistencies across documents | Human oversight to prevent false positives |
Algorithmic decision-making tools may incorporate biases present in training data or may produce disparate impacts on protected groups. Under Title VII and similar anti-discrimination laws, employment practices that produce disparate impact on protected classes may violate legal requirements even without intentional discrimination. Healthcare organizations considering AI-enabled screening tools should evaluate whether tools have been tested for bias and disparate impact, whether they satisfy applicable validation requirements, and whether decision processes are sufficiently transparent to permit meaningful review and explanation.
Regulatory frameworks governing AI use in employment decisions remain in development. Some jurisdictions have begun implementing requirements for algorithm auditing, impact assessment, or notice to applicants when automated systems influence hiring decisions.
Blockchain and Decentralized Credential Verification
Blockchain technology has been proposed as a method for credential verification, potentially enabling individuals to maintain verified credential records that employers can access with permission. Decentralized verification models could reduce redundant verification efforts when individuals move between employers and provide real-time credential status information.
Practical implementation faces challenges including adoption by licensing authorities and educational institutions, standardization across jurisdictions and professions, privacy and security safeguards, and integration with existing verification systems. Healthcare organizations should monitor developments in this area while maintaining conventional verification processes until decentralized systems achieve sufficient maturity and adoption.
Conclusion
Future-proofing healthcare screening programs for 2026 requires viewing screening as compliance architecture rather than administrative process. By integrating federal exclusion monitoring, state-specific requirements, and operational frameworks that address workforce dynamics, healthcare organizations build resilient systems that protect patient safety while supporting hiring objectives. Screening program design should involve legal and compliance review to ensure alignment with applicable requirements. Continuous adaptation to regulatory changes and workforce realities remains essential.
Frequently Asked Questions
In terms of the process of healthcare screening, it is not uncommon to wonder about the process, the scope, and the best way to align all of the federal, state, and operational needs into one process. Given the ever-changing landscape of regulations, as well as the increasingly complex workforce, it is understandable that there is a need to understand the process before moving forward with the overall approach. The following FAQs will address the concerns that many have with exclusion monitoring, license verification, continuous oversight, and documentation standards.
What makes healthcare screening programs different from general employment background checks?
Healthcare screening programs incorporate specialized components including federal exclusion database monitoring, professional license verification, abuse registry checks, and healthcare-specific disciplinary databases. These elements reflect regulatory requirements for Medicare and Medicaid participation, state healthcare facility licensing standards, and patient safety obligations that do not apply to general employment. Healthcare roles involve vulnerable populations and safety-sensitive responsibilities that necessitate more comprehensive verification than many other industries require.
How often should healthcare organizations check federal exclusion databases?
Federal guidance does not specify mandatory checking frequency, but healthcare organizations should implement monitoring sufficient to detect exclusions promptly and prevent excluded individuals from participating in federal healthcare programs. Many organizations conduct exclusion checks at hire and implement monthly monitoring thereafter. Some use continuous monitoring systems that check databases more frequently and generate immediate alerts when exclusions occur.
Do state-specific healthcare screening requirements apply to telehealth providers practicing across state lines?
Jurisdictional questions regarding telehealth providers remain complex, as both the state where the provider is located and states where patients receive care may assert regulatory authority. Healthcare organizations offering telehealth services should evaluate screening requirements in states where providers are licensed, where the organization operates, and where patients are located. Requirements vary by state, and legal frameworks governing interstate telehealth practice continue to evolve.
What is the difference between point-in-time screening and continuous monitoring?
Point-in-time screening verifies background information at a specific moment, typically at hire, but provides no ongoing oversight of subsequent developments. Continuous monitoring involves regular automated checking of databases to detect new information such as exclusions, license suspensions, or disciplinary actions that occur after initial screening. Continuous monitoring enables prompt response to changes affecting employment eligibility or patient safety.
How should healthcare organizations handle screening for contract or agency staff?
Healthcare organizations maintain regulatory responsibility for patient safety and federal healthcare program participation requirements even when engaging workers through staffing agencies. Organizations should establish minimum screening standards that agencies must meet and require documentation demonstrating compliance with those standards. Contractual agreements should specify screening requirements, documentation expectations, and ongoing monitoring responsibilities.
What documentation should healthcare organizations maintain regarding employee screening?
Comprehensive documentation should identify screening components performed, databases searched, search dates, results obtained, and how results were interpreted. Records should demonstrate exclusion database checking frequency and results, license verification with license numbers and expiration dates, and any identified issues along with assessment processes and decisions. Documentation serves as compliance evidence during regulatory surveys or audits and supports quality improvement efforts.
Can healthcare organizations implement provisional employment while screening is completed?
Provisional employment arrangements permit individuals to begin work based on preliminary screening results while comprehensive checks are finalized. Policies should specify which critical safety checks, such as exclusion database searches and primary license verification, must be completed before work begins. If screening conducted during the provisional period reveals information that leads to termination or other adverse action, and that information was obtained through a consumer report, organizations must comply with Fair Credit Reporting Act requirements including pre-adverse action and adverse action notices.
How do ban-the-box laws affect healthcare hiring and background screening?
Ban-the-box laws restrict when employers may inquire about criminal history during hiring. Healthcare positions may qualify for exemptions in some jurisdictions based on patient safety considerations, but exemption availability and scope vary by location. Healthcare organizations must determine which positions qualify for exemptions, when criminal history inquiries and screening may occur, and how to conduct individualized assessments when criminal history is identified.
Additional Resources
- Office of Inspector General List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/ - System for Award Management Exclusions
https://sam.gov/content/exclusions - Federation of State Medical Boards
https://www.fsmb.org/ - National Practitioner Data Bank
https://www.npdb.hrsa.gov/ - Centers for Medicare and Medicaid Services Compliance Resources
https://www.cms.gov/priorities/key-initiatives/burden-reduction/administrative-simplification/compliance

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.