Healthcare organizations face unprecedented challenges balancing rapid gig worker onboarding with comprehensive background screening requirements in 2025. This guide provides healthcare HR directors and compliance officers with actionable frameworks to maintain regulatory compliance while efficiently integrating temporary workers, traveling nurses, and medical contractors into their staffing models.
Key Takeaways
- Healthcare gig worker background checks must meet rigorous standards including FBI fingerprinting, OIG exclusion searches, and state-specific medical licensing verification.
- Standard healthcare background screening takes 7-14 days, but expedited services reduce turnaround to 48-72 hours without compromising compliance.
- FCRA compliance requires proper disclosures, written authorization, and adverse action procedures even for short-term gig assignments.
- Multi-state licensing verification is critical as 45% of healthcare gig workers operate across state lines, requiring checks in each jurisdiction.
- Continuous monitoring programs identify credential expirations, license suspensions, and exclusion list additions in real-time.
- Technology platforms integrating API-based verification systems reduce administrative burden by 60% while improving screening accuracy.
- Non-compliance with healthcare background check requirements can result in penalties ranging from $25,000 to $1.1 million per violation.
Types of Healthcare Gig Workers Requiring Background Checks
The healthcare gig economy encompasses diverse worker categories, each requiring tailored background screening approaches. Understanding these distinctions helps organizations apply appropriate verification protocols. The specific screening depth varies based on patient contact level, prescriptive authority, and controlled substance access.
Healthcare organizations must recognize that all gig worker categories require comprehensive background checks regardless of assignment duration. The following categories represent the most common healthcare gig worker types requiring verification:
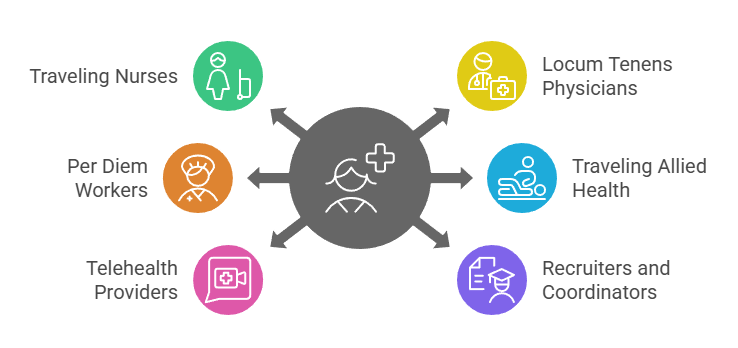
- Traveling Nurses (RNs and LPNs): Contract nurses working temporary assignments across multiple facilities or states, typically for 13-week periods, requiring multistate license verification and continuous credential monitoring.
- Locum Tenens Physicians: Temporary physicians filling staffing gaps in hospitals and clinics, requiring DEA verification, board certification confirmation, and malpractice insurance validation.
- Per Diem Healthcare Workers: On-call nurses, medical assistants, and patient care technicians working flexible shifts without guaranteed hours.
- Traveling Allied Health Professionals: Physical therapists, respiratory therapists, radiology technologists, and occupational therapists on temporary assignments requiring state-specific license verification.
- Telehealth Providers: Remote physicians, nurse practitioners, and mental health professionals providing virtual care requiring license verification in all states where patients are located.
- Healthcare Recruiters and Staffing Coordinators: Contract professionals managing temporary healthcare placement requiring background checks despite limited direct patient contact.
Organizations should establish clear classification criteria for each gig worker category specifying required background check components based on role responsibilities and regulatory requirements.
EXPERT INSIGHT: Today's health care environment is one of speed versus safety and I've discovered that the best part of being a health care leader is learning to stop at neither. It's not just a necessary check-the-box exercise to balance quick hiring with background checks. It's a moral imperative that protects patients, employees, and the care they receive. Every credential and background check is a story; a nurse transitioning to a new organization, a physician restoring their reputation, a patient looking to the unseen work. When HR acts with both speed and compassion at the heart of our decisions, we can hire to fulfill a role quickly, and we can build a strong health care foundation. Ultimately, proper health care requires not health care red-tape. It requires compassion. - Charm Paz, CHRP
Understanding Healthcare Gig Worker Background Check Requirements
The healthcare gig economy has expanded dramatically since 2020. Over 2.3 million temporary and contract medical workers now comprise approximately 15% of the total healthcare workforce in the United States. This surge has created complex compliance challenges for organizations.
They must apply the same stringent background screening standards to short-term workers that traditionally applied only to permanent employees. Healthcare organizations cannot compromise on thoroughness despite pressure to fill positions quickly. Regulatory bodies hold facilities accountable for credential verification regardless of employment classification.
The regulatory framework governing healthcare gig worker background checks encompasses multiple requirements. These include federal requirements from CMS and state health department mandates. They also include accreditation standards from The Joint Commission and FCRA provisions protecting worker rights.
Federal Compliance Standards for Medical Contractors
Federal regulations establish baseline requirements that apply regardless of state location or employment classification. CMS requires all healthcare facilities participating in Medicare or Medicaid to conduct comprehensive background checks. These checks include criminal history reviews and OIG exclusion list searches. They also include SAM verification to ensure workers haven't been barred from federal healthcare programs.
These searches must be completed before the worker provides patient care. They must be repeated monthly for exclusion lists to maintain continuous compliance. The FCRA imposes specific procedural requirements when healthcare organizations use consumer reporting agencies for background screening.
Non-compliance with FCRA provisions can result in statutory damages of $100-$1,000 per violation plus actual damages and attorney fees, creating significant financial exposure for healthcare staffing operations.
State-Specific Healthcare Temporary Worker Screening Variations
State requirements for healthcare temporary worker screening vary significantly across the country. California mandates FBI fingerprint-based background checks for certain healthcare positions and requires tuberculosis testing within the past year. Texas enforces Employee Misconduct Registry checks and abuse registry searches specific to healthcare settings.
Florida requires Level 2 background screening for healthcare practitioners with direct patient contact. This includes fingerprinting through the Florida Department of Law Enforcement and FBI databases. Healthcare organizations must identify the most stringent requirements across all jurisdictions and apply those standards uniformly to ensure compliance.
The following table outlines critical state-specific variations affecting traveling nurse background screening processes:
| State Requirements | Criminal History Lookback | License Verification | Additional Mandates |
| California | 7 years for most offenses | Real-time BRN verification | FBI fingerprinting, TB testing, abuse registry |
| Texas | No statutory limit | BON database + disciplinary actions | Employee Misconduct Registry, Nurse Aide Registry |
| Florida | No statutory limit | DOH license verification + NPDB | Level 2 FDLE + FBI fingerprinting |
| New York | Article 23-A consideration factors | OP.ED verification system | SCR abuse check, Justice Center background check |
Organizations managing healthcare gig workers across multiple states should establish standardized protocols meeting the highest common denominator of requirements.
Essential Components of Healthcare Contractor Background Checks
Comprehensive healthcare gig worker background checks comprise multiple verification layers. Each component serves a distinct compliance purpose. Healthcare organizations must complete all required elements before allowing gig workers to begin patient contact.
Documentation must be retained according to state-specific record retention requirements ranging from three to seven years post-assignment. The depth and breadth of these verification requirements reflect the critical nature of healthcare services and the vulnerable populations served.
Criminal History and Fingerprint-Based Screening
Criminal background checks for healthcare gig workers must extend beyond standard county or state searches. They must include FBI fingerprint-based verification, particularly for positions involving vulnerable populations or controlled substance access. Fingerprint-based screening provides the most accurate identification matching.
Thirty-seven states now mandate fingerprint background checks for at least some categories of healthcare workers. Twelve states require FBI channeling for all direct patient care positions. Healthcare organizations must establish clear adjudication standards considering offense type, severity, recency, and rehabilitation evidence.
The scope of criminal history review should include several key elements:

- County Criminal Searches: Court records from all counties where the worker has resided in the past 7-10 years provide the most current local offense information.
- Statewide Criminal Database Checks: Repository searches in all states of residence and employment.
- Federal Criminal Records: PACER searches for offenses prosecuted in federal courts, including healthcare fraud and controlled substance violations.
- Sex Offender Registry Searches: Multi-jurisdictional registry checks required in most states for healthcare workers with patient contact.
These comprehensive criminal screening measures protect both patients and healthcare organizations.
Professional License and Credential Verification
Medical contractor background check requirements include thorough validation of professional licenses, certifications, and educational credentials. Organizations must conduct verification through primary sources only. The Joint Commission standards mandate direct confirmation with issuing authorities.
This verification must confirm current active status and absence of disciplinary actions. It must also identify practice limitations and any conditions affecting scope of practice. For traveling nurses, license verification becomes particularly complex with the growing adoption of the Nurse Licensure Compact.
Professional credential verification should encompass active license status, disciplinary history review, DEA registration verification for prescribers, board certification confirmation, and educational verification requiring degree confirmation directly from institutions.
Exclusion Database and Sanctions Screening
Federal and state exclusion lists identify individuals prohibited from participating in government healthcare programs. These searches represent non-negotiable components of healthcare gig worker background checks. The OIG List of Excluded Individuals and Entities (LEIE) represents the primary federal database. Many states maintain separate Medicaid exclusion lists.
Employing excluded workers—even unknowingly—can result in severe consequences. Organizations face civil monetary penalties, program exclusion, and False Claims Act liability. Healthcare organizations must conduct exclusion searches before engagement and repeat these searches monthly throughout the assignment duration.
A single instance of billing federal healthcare programs for services provided by excluded individuals can trigger penalties ranging from $10,000-$50,000 per item or service. Organizations should implement centralized tracking systems that monitor all active gig workers against these databases with automated alerts.
Streamlining the Background Screening Process for Rapid Deployment

Healthcare organizations face intense pressure to onboard qualified gig workers quickly while maintaining comprehensive screening standards. The traditional background check timeline of 10-14 business days conflicts with urgent staffing needs. Delays of even 48 hours can compromise patient care quality and create operational bottlenecks.
Healthcare HR directors must implement strategic process improvements that reduce turnaround time without sacrificing thoroughness. Technology integration represents the most significant opportunity for accelerating healthcare gig worker background checks while improving accuracy.
Organizations using integrated background screening platforms report 60% faster turnaround times compared to traditional methods. These platforms provide automated status updates that give real-time visibility into pending verifications.
Implementing Expedited Healthcare Background Check Services
Expedited background screening services specifically designed for healthcare applications can compress standard timelines significantly. Standard processes taking 10-14 days can be reduced to 48-72 hours for most components. These services prioritize healthcare verifications and utilize direct electronic connections to data sources.
While expedited services typically cost 30-50% more than standard screening packages, the financial benefit often justifies the premium. Organizations avoid overtime costs and reduce agency markup expenses through faster placement.
The following verification timelines demonstrate acceleration potential:
- County Criminal Searches: 3-5 business days reduces to 24-48 hours through priority court runner service.
- FBI Fingerprinting: 7-10 business days compresses to 3-5 business days through Rapid Results channeling.
- License Verification: 1-3 business days reduces to same-day turnaround through real-time API connections.
- Exclusion Database Searches: Instant results through automated database queries.
- Employment Verification: 3-7 business days reduced to 24-72 hours through outsourced verification specialists.
Healthcare organizations should evaluate which positions truly require 48-hour deployment to control costs strategically.
FCRA Compliance for Healthcare Temporary Worker Screening
The Fair Credit Reporting Act governs background checks conducted through third-party consumer reporting agencies. FCRA violations have triggered significant penalties for healthcare employers, with settlement amounts ranging from $500,000 to $2.8 million in recent class-action cases.
Healthcare HR directors must understand that FCRA applies regardless of employment classification. Common FCRA compliance failures include bundling background check disclosures with other hiring documents, failing to obtain separate written authorization, and neglecting proper adverse action procedures.
The standalone disclosure requirement proves particularly problematic. Organizations cannot include liability waivers or other extraneous information on the same document where they disclose intent to obtain a background check.
Proper Disclosure and Authorization Procedures
Healthcare organizations must provide clear, standalone written disclosure before procuring background checks through consumer reporting agencies. This disclosure must appear in a document consisting solely of the disclosure stating that a consumer report may be obtained for employment purposes.
Following disclosure, organizations must obtain written authorization from the healthcare gig worker explicitly permitting the background check. While authorization may appear on the same document as disclosure, it cannot include waiver language.
Best practices for FCRA-compliant disclosure and authorization include:
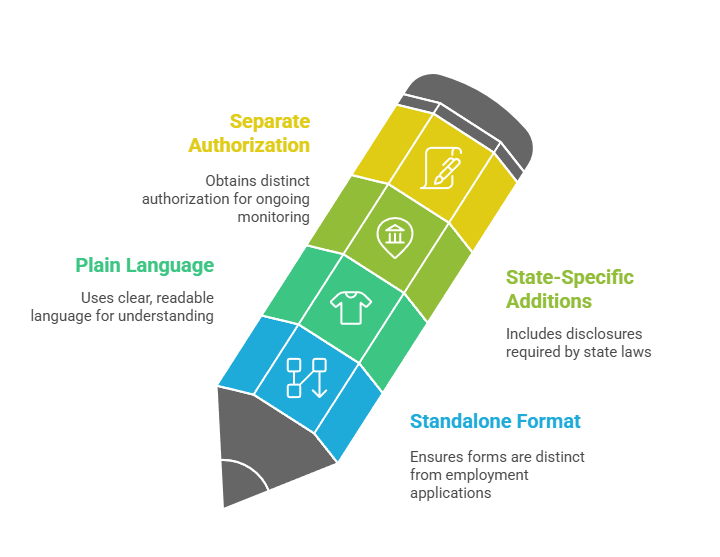
- Standalone Format: Create dedicated forms separated physically and visually from employment applications.
- Plain Language: Use clear, readable language at 8th-10th grade level explaining what information will be obtained.
- State-Specific Additions: Incorporate additional disclosures required by state laws such as California's ICRAA.
- Separate Authorization for Ongoing Monitoring: Obtain distinct authorization for continuous background monitoring programs.
Healthcare organizations should review disclosure documents annually with employment law counsel to ensure continued compliance.
Adverse Action Requirements and Candidate Rights
When healthcare organizations decide to disqualify gig workers based on background check findings, FCRA mandates a specific adverse action process. Organizations must provide pre-adverse action notice including a copy of the consumer report and the FTC's "Summary of Your Rights Under the Fair Credit Reporting Act."
The pre-adverse action waiting period should extend at least five business days to provide reasonable opportunity for candidates to respond with dispute information. Healthcare organizations that immediately finalize adverse decisions violate FCRA requirements.
After the waiting period concludes, final adverse action notice must be provided including specific information about the consumer reporting agency and notice of rights to dispute report accuracy.
Technology Solutions for Healthcare Gig Workforce Compliance
Healthcare organizations managing significant gig worker populations increasingly rely on integrated technology platforms. These systems automate background screening workflows and track compliance deadlines. They reduce administrative burden on HR staff by 50-70% compared to manual tracking methods.
Modern healthcare credentialing platforms integrate background checks with license verification, continuing education tracking, and competency assessment in unified systems. API-based integration enables real-time data exchange between screening providers, licensing boards, and healthcare organization systems.
Organizations implementing API-connected screening platforms report 85% faster turnaround for license verification and exclusion searches compared to manual lookups.
Automated Continuous Monitoring Systems
Continuous monitoring technology automatically rescreens active healthcare gig workers on scheduled intervals. The system checks against criminal databases, exclusion lists, and licensing boards, alerting compliance officers immediately when adverse changes occur.
CMS increasingly expects healthcare organizations to implement continuous monitoring, particularly for workforce segments with higher turnover. Monthly exclusion list checks and quarterly license/criminal monitoring represent minimum standards for healthcare workers.
These systems should provide comprehensive functionality:
- Multi-Database Coverage: Simultaneous monitoring of federal/state exclusion lists, licensing boards, and national criminal databases.
- Instant Alert Notifications: Real-time notifications to compliance officers when monitoring identifies adverse changes.
- Audit Documentation: Comprehensive logging of all monitoring activities and findings for regulatory audits.
- Worker Self-Service Portals: Platforms allowing gig workers to view their background check status and upload credential renewals.
Even a single instance of employing an excluded worker can trigger penalties exceeding annual monitoring costs for an entire gig workforce.
Integration with Healthcare Staffing Management Platforms
Modern vendor management systems and healthcare-specific staffing platforms increasingly incorporate background screening as integrated workflow components. They enable healthcare organizations to requisition gig workers, automatically initiate appropriate background checks, and track verification status—all within unified systems.
Integration eliminates double data entry and reduces processing time by 40-60%. Healthcare staffing agency compliance requirements become more manageable when background screening integrates with placement workflows. Agencies can demonstrate that all placed workers have completed required verifications before assignment.
Managing Multi-State Healthcare Gig Worker Credentialing
Healthcare organizations utilizing traveling nurses and medical contractors across state lines face exponentially more complex background screening requirements. Each state maintains distinct licensing requirements, background check mandates, and regulatory standards.
The Nurse Licensure Compact has simplified multi-state practice for RNs and LPNs, but significant verification complexities remain for non-compact practitioners. Multi-state credentialing requires organizations to identify the most stringent requirements across all practice jurisdictions and apply those standards uniformly.
Healthcare HR directors should establish state requirement matrices documenting specific background check components, lookback periods, acceptable verification sources, and renewal frequencies for each jurisdiction.
Nurse Licensure Compact Verification Requirements
The enhanced Nurse Licensure Compact allows registered nurses and licensed practical nurses to hold one multistate license with privilege to practice in all 41 compact member states. However, organizations must understand that compact licensure doesn't eliminate background check requirements.
Nurses must meet uniform licensure requirements including completion of FBI fingerprint background checks in their primary state of residence. Healthcare organizations employing compact license holders should verify the primary state of residence license and privilege-to-practice status.
Organizations must verify that no compact states have imposed practice restrictions and track any changes in the nurse's primary state of residence, which requires obtaining a new multistate license within 60 days.
Allied Health Professional Multi-State Requirements
Allied health professionals including respiratory therapists, radiology technologists, and physical therapists lack uniform interstate compacts in most disciplines. They require separate state licenses for each practice jurisdiction. Medical contractor background check requirements become particularly complex for professionals working in multiple states simultaneously.
Healthcare staffing agencies managing multi-state allied health contractors should implement comprehensive verification protocols covering state licensure determination, temporary/limited license tracking, and continuing education requirements.
The lack of standardization across states creates a significant administrative burden. Some allied health professionals maintain 5-8 separate state licenses simultaneously. Technology platforms that centralize multi-state license tracking become essential tools.
Cost Optimization Strategies for Healthcare Background Screening
Healthcare organizations face significant background screening expenses as gig worker populations expand. Comprehensive checks for traveling nurses and medical contractors range from $150-$400 per worker. Organizations managing 100+ gig workers annually can incur $40,000-$80,000 in direct background check costs.
Strategic cost management approaches can reduce these expenses by 30-40% without compromising thoroughness. Volume pricing arrangements with background screening providers offer the most direct cost reduction opportunity. Providers typically offer tiered pricing with discounts ranging from 15% at 100 annual checks to 35-40% at 500+ annual checks.
Organizations should negotiate comprehensive service agreements establishing clear turnaround time expectations, verification standards, and FCRA compliance guarantees.
Building Collaborative Screening Consortiums
Healthcare organizations within the same geographic region can realize significant economies of scale by establishing collaborative background screening consortiums. These arrangements aggregate volume across multiple facilities, enabling smaller hospitals to access enterprise-level pricing.
Consortiums typically negotiate master service agreements with screening providers and establish standardized verification protocols meeting all member requirements. Organizations participating in successful consortiums report 25-35% cost reductions compared to independent vendor relationships.
Legal counsel should review consortium arrangements to ensure appropriate data sharing agreements, liability provisions, and compliance with antitrust regulations.
Strategic Component Selection and Risk-Based Screening
Not all healthcare gig workers require identical background check depth. Organizations can establish tiered screening packages applying comprehensive checks to high-risk roles while using streamlined verification for lower-risk positions. This approach reduces average per-worker costs by 20-30%.
Risk-based screening frameworks generally classify roles into three tiers. The first tier involves comprehensive screening for positions with direct patient care and controlled substance access. This includes FBI fingerprinting, a 10-year criminal history review, and full credential verification. The second tier covers standard screening for roles with patient contact but no access to controlled substances, while the third tier applies basic screening to administrative staff with limited or no patient interaction.
Organizations should document position classifications and screening tier assignments to ensure appropriate risk mitigation while optimizing costs.
Conclusion
Healthcare gig worker background checks require organizations to balance urgent staffing needs with comprehensive compliance obligations. The strategies outlined in this guide enable healthcare HR directors to build efficient verification workflows incorporating proper FCRA procedures, multi-state credential management, and technology-enabled continuous monitoring. As the healthcare gig economy continues expanding in 2025 and beyond, organizations that master this compliance complexity will gain competitive advantage while minimizing regulatory and reputational risk. More importantly, because screening practices continue to ensure that patients and professionals are not harmed as a means to achieve compliance, it is always important to note that patient care and compliance can never work against each other. It is therefore vital to ensure that background screening is part of the duty of care of health care institutions.
Frequently Asked Questions
How long does a typical healthcare gig worker background check take?
Standard healthcare background checks take 7-14 business days to complete all required components. Expedited services can reduce this timeline to 48-72 hours for urgent staffing needs. The FBI fingerprinting component typically represents the longest verification element, requiring 5-10 business days through standard channels.
What background check components are legally required for traveling nurses?
Traveling nurses must complete criminal history checks covering all residence jurisdictions, state nursing license verification with disciplinary history review, and federal/state healthcare exclusion list searches. Most states additionally require fingerprint-based FBI background checks. Organizations must also verify BLS/ACLS certifications and specialty certifications relevant to assignment areas.
Are healthcare staffing agencies or client facilities responsible for background checks?
Legal responsibility for background check compliance ultimately rests with the healthcare facility where services are provided. However, most healthcare staffing agencies conduct initial background screening and maintain current credentials for placed workers. Best practice involves clear contractual delineation of screening responsibilities with agencies providing comprehensive verification documentation.
How often should exclusion list searches be repeated for active gig workers?
Federal guidance from the OIG requires monthly exclusion database searches for all active workforce members including temporary workers. This monthly cadence ensures organizations identify newly excluded individuals before submitting claims to federal healthcare programs. Automated continuous monitoring systems eliminate manual search burden while providing immediate alerts.
What are penalties for employing healthcare gig workers without proper background checks?
Healthcare organizations face civil monetary penalties of $10,000-$50,000 per claim for services by improperly credentialed workers. State health departments impose additional penalties from $1,000-$25,000 per violation. Organizations also face False Claims Act liability with treble damages and FCRA penalties of $100-$1,000 per violation.
Do FCRA requirements apply to healthcare gig workers differently than employees?
FCRA requirements apply identically to all employment-related background checks regardless of worker classification. Healthcare organizations must provide standalone written disclosure, obtain separate authorization, and follow adverse action procedures. Brief working relationships do not eliminate FCRA compliance obligations.
Can healthcare organizations share background check results between facilities?
Healthcare organizations can share results through portable credentialing programs or consortium arrangements when appropriate authorization exists. Sharing requires written worker authorization permitting credential disclosure to affiliated facilities. The Joint Commission platforms facilitate legitimate results sharing, though each facility retains responsibility for verifying information that meets their requirements.
What background check lookback periods apply to healthcare gig workers?
Federal law does not establish uniform lookback periods for healthcare workers, but FCRA restricts most criminal convictions to seven years. Many states prohibit these limitations for healthcare positions, requiring unlimited lookback for patient safety-relevant convictions. Healthcare organizations should conduct reviews covering at least 7-10 years.
Additional Resources
- OIG List of Excluded Individuals and Entities (LEIE) - Official Database
https://oig.hhs.gov/exclusions/ - The Joint Commission Standards for Healthcare Credentialing
https://www.jointcommission.org/standards/standard-faqs/hospital-and-hospital-clinics/human-resources-hr/000001455/ - Enhanced Nurse Licensure Compact (eNLC) State Participation Guide
https://www.ncsbn.org/nurse-licensure-compact.htm - Federal Trade Commission FCRA Guidance for Employment Screening
https://www.ftc.gov/business-guidance/resources/using-consumer-reports-what-employers-need-know - CMS Background Check Requirements for Healthcare Workers
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-17.pdf - National Practitioner Data Bank Guidebook for Healthcare Entities
https://www.npdb.hrsa.gov/resources/NPDBGuidebook.pdf - EEOC Guidance on Arrest and Conviction Records in Employment Decisions
https://www.eeoc.gov/laws/guidance/enforcement-guidance-consideration-arrest-and-conviction-records-employment-decisions

