FACIS® (Fraud and Abuse Control Information System) background checks are specialized screenings that search federal databases for healthcare practitioners excluded from participating in federal healthcare programs. These checks provide critical risk mitigation for medical employers who must verify that candidates are eligible to provide services reimbursed by Medicare, Medicaid, and other government healthcare programs. Proper FACIS screening protects healthcare organizations from substantial financial penalties, operational disruptions, and reputational damage while ensuring patient safety through comprehensive credential verification.
Key Takeaways
- FACIS® background checks search the OIG List of Excluded Individuals and Entities (LEIE) and the SAM.gov exclusion database to identify healthcare workers barred from federally funded programs, making this screening legally mandatory for healthcare employers participating in Medicare or Medicaid.
- Healthcare organizations face potential penalties including loss of federal funding, substantial fines, and program exclusion if they employ individuals listed in FACIS databases, creating significant financial and operational risks beyond standard employment violations.
- FACIS screening differs fundamentally from traditional criminal background checks by focusing specifically on federal healthcare program exclusions, professional sanctions, and credential-related fraud rather than general criminal history.
- Healthcare employers must conduct FACIS checks before hiring and implement ongoing monthly monitoring to remain compliant, as exclusions can occur at any time during employment due to newly discovered violations or license actions.
- The FACIS verification process integrates with professional license verification and creates a comprehensive healthcare-specific screening framework that addresses the unique regulatory requirements of medical practice environments.
- Healthcare job seekers should proactively verify their own FACIS status before applying for positions in medical settings, as exclusions can result from administrative actions, civil settlements, or professional license issues unrelated to criminal convictions.
- Implementing automated FACIS monitoring systems reduces administrative burden and compliance risk by providing real-time alerts when current employees appear on exclusion lists, enabling immediate remediation before audit exposure.
- Healthcare organizations must develop clear adverse action protocols that comply with both FCRA requirements and healthcare-specific regulations when FACIS screenings reveal exclusionary information that impacts hiring or employment decisions.
Understanding FACIS® Background Checks in Healthcare Employment
FACIS background checks represent a specialized category of employment screening designed exclusively for healthcare industry hiring. Unlike general criminal background checks that examine court records and criminal history, FACIS searches query federal databases maintained by the Office of Inspector General (OIG) and the General Services Administration (GSA). These searches identify individuals and entities excluded from participating in federal healthcare programs.
The term FACIS historically referenced a proprietary database system. Today, healthcare employers primarily access two critical public databases: the OIG List of Excluded Individuals and Entities (LEIE) and the System for Award Management (SAM.gov) exclusion records. These databases contain records of healthcare practitioners, suppliers, and organizations that have been sanctioned, excluded, or debarred from receiving payments from Medicare, Medicaid, TRICARE, and other federally funded healthcare programs.
Healthcare employers who participate in federal healthcare programs face strict legal obligations to verify that employees, contractors, and vendors do not appear on these exclusion lists. Consequences of employing excluded individuals extend far beyond standard employment law violations. Organizations risk losing Medicare and Medicaid participation privileges, facing substantial civil monetary penalties, and experiencing federal program exclusion that could prove financially catastrophic.
EXPERT INSIGHT: By observing how screening and compliance functions, I have learned that background screening is not simply a policy issue, it is also a way to maintain integrity not just in a company, but also among those they serve. I have observed how a small discrepancy may escalate into a potentially stressful situation that could have been avoided. On the other hand, every outcome is tied to a person who should get a clear answer. - Charm Paz, CHRP
Why Healthcare Background Checks Require Specialized Screening
The healthcare industry operates under a significantly more complex regulatory framework than most other employment sectors. Federal and state agencies impose specific screening requirements that reflect the unique vulnerabilities inherent in medical practice environments. Practitioners access sensitive patient information, controlled substances, and vulnerable populations while providing care that directly impacts health outcomes.
Healthcare background screening must address multiple risk dimensions simultaneously:

- Professional licensure verification: Confirming active, unrestricted licenses appropriate to practice scope
- Federal exclusion database checks: Searching LEIE and SAM.gov for program participation bars
- Criminal history verification: Identifying disqualifying offenses related to patient safety and program integrity
- Educational credential validation: Verifying degrees, certifications, and clinical training credentials
- Clinical privileges confirmation: Checking hospital privileges and specialty board certifications
This multi-layered verification process reflects the heightened duty of care healthcare organizations owe to patients. Extensive regulatory oversight governing medical practice creates compliance obligations that exceed those in non-healthcare employment sectors.
The Legal Framework Mandating FACIS® Verification
Federal healthcare program participation requirements establish clear obligations for healthcare employers to screen potential and current employees against exclusion databases. Section 1128 of the Social Security Act authorizes the OIG to exclude individuals and entities from federal healthcare programs based on various grounds. These grounds include Medicare or Medicaid fraud, patient abuse, felony convictions related to healthcare, and license revocation or suspension by state licensing authorities.
Healthcare organizations that employ excluded individuals may face civil monetary penalties under the Civil Monetary Penalties Law (CMPL). The OIG may impose penalties for each item or service furnished by an excluded individual, with amounts reaching thousands of dollars per violation. Additionally, the employing organization risks exclusion from federal healthcare programs, which would effectively terminate its ability to receive Medicare and Medicaid reimbursement.
| Violation Type | Potential Penalty | Additional Consequences |
| Employing excluded individual | Up to $10,000 per item/service | Loss of federal program participation |
| Failure to verify exclusion status | Civil monetary penalties | Heightened audit scrutiny |
| Submitting claims for excluded provider services | Treble damages + penalties | Corporate Integrity Agreement requirements |
The Centers for Medicare and Medicaid Services (CMS) require healthcare organizations to implement screening protocols as a condition of program participation. While CMS does not mandate specific screening methodologies, compliance standards established through OIG guidance make clear expectations. Organizations must check the LEIE and SAM.gov databases before hiring and implement ongoing monthly monitoring of current employees, contractors, and vendors.
How FACIS® Background Checks Work
The FACIS screening process involves querying federal exclusion databases to determine whether a healthcare worker or organization appears on lists maintained by the OIG or GSA. Healthcare employers can access these databases directly through free public search portals. Alternatively, organizations may utilize third-party screening services that automate the verification process and provide ongoing monitoring capabilities.
The OIG maintains the List of Excluded Individuals and Entities (LEIE) at oig.hhs.gov, providing a searchable database of all individuals and entities currently excluded from participating in Medicare, Medicaid, and other federal healthcare programs. Database entries include identifying information such as names, addresses, dates of birth, and exclusion details. Exclusion details specify the basis for exclusion, the excluding agency, and the exclusion period.
The SAM.gov system, managed by the General Services Administration, consolidates multiple federal exclusion lists into a single searchable database:
- Healthcare-specific exclusions: OIG program exclusions for fraud, abuse, and license actions
- Federal contracting debarments: GSA exclusions for contract-related violations
- Cross-program suspensions: Exclusions affecting multiple federal benefit programs
- State Medicaid exclusions: State-level program participation bars reported to federal databases
While SAM.gov includes broader federal contracting exclusions beyond healthcare-specific sanctions, healthcare employers should search this database because it contains exclusion records that may not appear in the LEIE. Records related to federal contracting debarments or non-healthcare federal program violations require separate verification.
The Screening Implementation Process
Healthcare organizations implementing FACIS screening should establish clear protocols that define when screenings occur, who conducts the searches, and how results are documented. Best practices include conducting FACIS checks during the pre-employment phase, before extending conditional job offers. Early screening avoids the operational disruptions and potential liability associated with rescinding offers or terminating newly hired employees.
The verification process requires collecting sufficient identifying information from candidates to conduct accurate database searches. Healthcare employers must obtain proper authorization from candidates before conducting these verifications. Organizations must follow Fair Credit Reporting Act (FCRA) requirements when screenings are performed by third-party consumer reporting agencies.
Integrating FACIS® Screening with Comprehensive Healthcare Background Checks
FACIS verification represents one component of a comprehensive healthcare background screening program. Healthcare employers should implement multi-layered verification protocols that address all relevant risk dimensions while maintaining operational efficiency. Candidate experience standards must balance thoroughness with reasonable timelines.
| Screening Component | Primary Purpose | Typical Timeline |
| FACIS database search | Federal program eligibility verification | 1-2 business days |
| Professional license verification | Active licensure and discipline check | 2-3 business days |
| Criminal background check | Safety and suitability assessment | 3-5 business days |
| Employment history verification | Experience and credential validation | 5-7 business days |
| Education credential verification | Degree and certification confirmation | 7-10 business days |
Professional license verification forms a critical parallel screening component. Healthcare employers must confirm that practitioners hold active, unrestricted licenses appropriate to their practice scope. License verification involves checking state licensing board databases to confirm license status, verify that no disciplinary actions or restrictions limit practice authority, and ensure that licensure covers the specific practice location and service types.
Criminal Background Checks in Healthcare Settings
Criminal background checks remain essential for healthcare hiring despite the specialized nature of FACIS screening. Healthcare employers must verify that candidates possess no disqualifying criminal history. Particular attention should focus on offenses involving violence, theft, fraud, controlled substances, or crimes against vulnerable individuals.
Healthcare organizations should develop clear criminal background check policies that define disqualifying offenses and establish individualized assessment procedures. Policies must comply with applicable federal, state, and local regulations. The FCRA requires employers to follow specific adverse action procedures when criminal background information influences employment decisions.
Ongoing Monitoring Requirements and Best Practices
Healthcare organizations' FACIS screening obligations extend beyond pre-employment verification. The OIG can add individuals and entities to exclusion lists at any time based on newly discovered violations, recent convictions, or license actions that trigger mandatory exclusion authorities. Healthcare employers who fail to detect mid-employment exclusions face the same penalties and consequences as those who hire initially excluded individuals.
Best practice guidance recommends monthly monitoring of all employees, contractors, and vendors against the LEIE and SAM.gov databases. This ongoing screening protocol ensures that healthcare organizations identify exclusions promptly. Organizations can then take immediate remediation actions to prevent claims submission for services rendered by excluded individuals.
Monthly monitoring creates several operational requirements:
- Automated query systems: Technology platforms that search exclusion databases regularly without manual intervention
- Alert mechanisms: Immediate notifications when current workforce members appear on exclusion lists
- Response protocols: Clear procedures defining actions when mid-employment exclusions are identified
- Documentation standards: Comprehensive records of all monitoring activities and exclusion investigations
- Audit preparation: Organized evidence demonstrating compliance with ongoing screening obligations
Manual monthly monitoring presents significant administrative challenges for healthcare organizations with large workforces or high employee turnover. Searching databases individually for each employee consumes substantial staff time and creates opportunities for human error or oversight. Many healthcare organizations implement automated monitoring systems that query exclusion databases regularly and generate alerts when current employees appear on exclusion lists.
Responding to Mid-Employment Exclusions
When ongoing monitoring identifies that a current employee has been added to a federal exclusion list, healthcare organizations must act immediately to prevent further violations. The employee should be removed from any roles involving federal healthcare program participation. This typically means immediate suspension or termination for most healthcare practitioners whose primary job functions involve providing reimbursable services.
Healthcare organizations should establish clear policies defining response protocols when exclusions are identified. Organizations must balance compliance obligations with employment law considerations. Adverse actions based on exclusion status must follow proper procedural requirements and maintain appropriate documentation.
FACIS® Compliance for Different Healthcare Settings

FACIS screening requirements apply consistently across healthcare settings that participate in federal healthcare programs. Implementation approaches may vary based on organizational structure, workforce composition, and operational models. Each healthcare setting faces unique challenges in establishing and maintaining compliant screening protocols.
Hospitals and large healthcare systems typically develop centralized screening protocols managed by human resources departments or compliance offices. These organizations often implement enterprise-wide automated monitoring systems that provide consistent screening coverage across multiple facilities and employment categories. Large healthcare employers may conduct FACIS screenings internally using direct database access or contract with third-party screening providers that offer comprehensive healthcare background check services.
Small medical practices and ambulatory care clinics face similar compliance obligations but may lack dedicated compliance resources. These organizations can access LEIE and SAM.gov databases directly through free public portals. Manual screening processes require establishing clear protocols for documenting search results and maintaining verification records.
| Healthcare Setting | Screening Frequency | Special Requirements |
| Hospitals | Pre-hire + monthly monitoring | Medical staff credentialing integration |
| Nursing homes | Pre-hire + monthly + state-mandated fingerprinting | Vulnerable population protection protocols |
| Home health agencies | Pre-hire + monthly for all contractors | Independent contractor screening obligations |
| Ambulatory surgery centers | Pre-hire + monthly | State facility licensing requirements |
| Medical practices | Pre-hire + monthly monitoring | Professional liability insurance verification |
Long-term care facilities and home health agencies face particularly stringent screening requirements due to their service focus on vulnerable elderly populations. Many states impose additional criminal background check requirements beyond federal FACIS screening for nursing home employees and home health workers.
Understanding Exclusion Bases and Healthcare Risk Factors
The OIG excludes individuals and entities from federal healthcare program participation based on various statutory authorities. Understanding common exclusion bases helps healthcare employers assess risk factors during hiring. Organizations can develop appropriate screening protocols that address the most prevalent exclusion scenarios.
Mandatory exclusions under Section 1128(a) of the Social Security Act apply to individuals convicted of program-related crimes, patient abuse or neglect, or felony convictions related to healthcare fraud. These mandatory exclusions carry minimum five-year exclusion periods, though many extend significantly longer depending on aggravating factors. Healthcare employers cannot employ mandatorily excluded individuals in any capacity involving federal program participation during the exclusion period.
Permissive exclusions under Section 1128(b) address a broader range of violations:
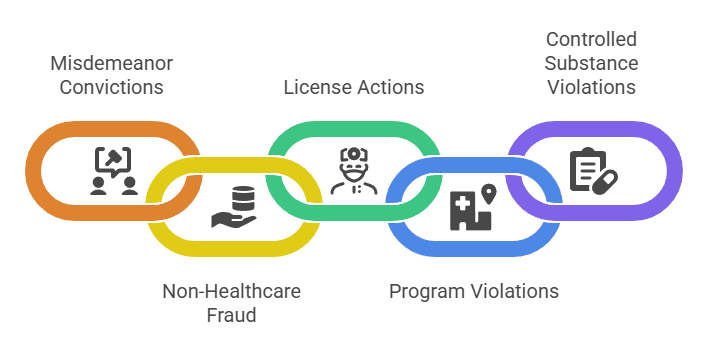
- Misdemeanor convictions: Healthcare-related offenses that do not rise to felony level
- Non-healthcare fraud: Violations involving other federal or state programs
- License actions: Revocation, suspension, or surrender based on professional misconduct
- Program violations: Exclusion or suspension from other federal or state healthcare programs
- Controlled substance violations: Convictions related to prescription drug offenses
Healthcare practitioners may face OIG exclusion based on state licensing board actions even when no criminal conviction has occurred. License revocation, suspension, or surrender based on professional misconduct, impairment, or quality of care issues may trigger federal exclusion authorities.
Adverse Action Procedures for FACIS-Based Employment Decisions
When FACIS screening reveals that a candidate or employee appears on federal exclusion lists, healthcare employers must implement proper adverse action procedures. Procedures must comply with applicable employment laws while addressing urgent compliance obligations. Healthcare organizations face unique challenges balancing legal requirements with immediate patient safety and program integrity concerns.
The Fair Credit Reporting Act requires specific procedural steps when employers take adverse actions based on information obtained from consumer reports. If FACIS screening is conducted by a third-party consumer reporting agency, healthcare employers must provide pre-adverse action notices. Notices must include a copy of the consumer report and a summary of FCRA rights before taking final adverse action.
| Scenario | Immediate Action | FCRA Requirement | Timeline |
| Pre-employment exclusion identified | Withdraw conditional offer | Pre-adverse notice + 5-day waiting period | 5-7 business days |
| Current employee newly excluded | Immediate suspension from federal program services | Post-termination adverse notice if CRA used | Within 24-48 hours |
| Contractor exclusion discovered | Immediate contract suspension | Contract terms govern notice requirements | Immediate |
Healthcare employers should develop clear policies that define decision-making protocols when exclusions are identified. While federal program participation requirements effectively mandate automatic disqualification for most healthcare roles, clear policies prevent inconsistent application and support defensible employment decisions.
Implementation Guidance for Healthcare Employers
Healthcare organizations implementing or enhancing FACIS screening programs should begin by conducting comprehensive compliance assessments. Assessments should identify current screening practices, document gaps relative to federal requirements, and establish clear implementation priorities. Organizations must allocate appropriate resources to maintain sustainable compliance programs.
Policy development should address key operational questions:
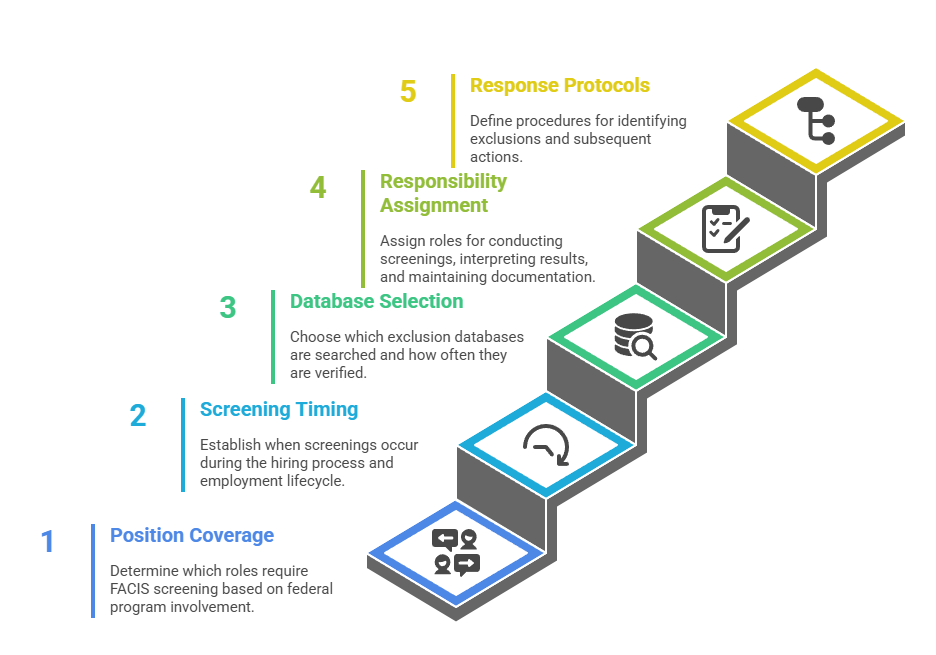
- Position coverage: Which roles require FACIS screening based on federal program involvement
- Screening timing: When screenings occur during the hiring process and employment lifecycle
- Database selection: Which exclusion databases are searched and verification frequency
- Responsibility assignment: Who conducts screenings, interprets results, and maintains documentation
- Response protocols: What procedures govern identification of exclusions and subsequent actions
Written policies create consistency, support staff training, and demonstrate compliance commitment during audits or investigations. Healthcare employers should establish clear documentation protocols that maintain records of all FACIS screenings and ongoing monitoring activities.
FACIS® Screening Considerations for Healthcare Job Seekers
Healthcare job seekers should understand that FACIS screening represents a standard component of hiring processes for positions in medical practice settings. Proactive steps can help candidates prepare for screenings and address potential issues before they impact employment opportunities. Understanding the screening process enables job seekers to gather necessary documentation and respond appropriately to employer verification requests.
Healthcare practitioners should periodically verify their own exclusion status by searching the LEIE and SAM.gov databases. These free public databases allow individuals to confirm that no exclusion records appear under their names. Practitioners who identify unexpected exclusion records should investigate immediately to determine whether the records represent actual exclusions or erroneous matches to individuals with similar names.
Individuals who have been excluded from federal healthcare programs should understand the reinstatement process and requirements for program eligibility restoration. The OIG exclusion authorities page provides guidance on requesting reinstatement after exclusion periods expire. Reinstatement is not automatic; excluded individuals must submit formal reinstatement requests and demonstrate that the factors leading to exclusion have been resolved.
Conclusion
FACIS background checks provide essential verification that healthcare workers remain eligible to participate in federal healthcare programs, protecting organizations from substantial penalties while supporting patient safety objectives. Healthcare employers must implement comprehensive screening protocols that include pre-employment FACIS verification and ongoing monthly monitoring. Also essential is the consistent application and communication of such processes to both job seekers and employees. When this screening is carried out with diligence and attention to detail, it improves integrity and trust within the health workforce.
Frequently Asked Questions
What is a FACIS background check and why is it required for healthcare employment?
A FACIS® background check searches federal databases maintained by the Office of Inspector General and the General Services Administration to determine whether healthcare workers appear on exclusion lists that bar participation in Medicare, Medicaid, and other federal healthcare programs. Healthcare employers who participate in federal programs face legal obligations to verify that employees are not excluded, as employing excluded individuals can result in substantial penalties and loss of federal funding. This screening requirement reflects federal program integrity protections designed to prevent individuals who have committed healthcare fraud or abuse from participating in federally funded healthcare delivery.
How often should healthcare employers conduct FACIS screenings on current employees?
Healthcare organizations should conduct FACIS screenings before hiring and implement ongoing monthly monitoring of all current employees, contractors, and vendors who participate in roles involving federal healthcare program services. Monthly monitoring represents the industry standard recommended by compliance experts and supported by OIG guidance. This frequency ensures that organizations identify mid-employment exclusions promptly and can take immediate corrective actions before submitting claims for services provided by excluded individuals.
Can healthcare workers be excluded from federal programs without being convicted of crimes?
Yes, healthcare practitioners may face OIG exclusion based on license revocations or suspensions by state licensing boards, civil settlements involving fraud allegations, or administrative violations even when no criminal conviction has occurred. The Social Security Act authorizes both mandatory and permissive exclusions covering a range of conduct beyond criminal convictions. Healthcare job seekers should understand that exclusion list appearance does not necessarily indicate criminal activity, though exclusions create the same federal program participation bars regardless of the underlying basis.
What happens if a healthcare employer discovers a current employee on a federal exclusion list?
Healthcare organizations that identify current employees on federal exclusion lists must take immediate action to prevent the excluded individual from providing federally reimbursable services, which typically requires immediate suspension or termination. The organization should document the exclusion discovery, suspend or terminate the employee following proper adverse action procedures, and review claims submitted during any period of unknowing exclusion. Employers cannot continue employing excluded individuals in federally funded roles even during exclusion disputes.
Are FACIS background checks the same as criminal background checks?
No, FACIS background checks serve a distinct purpose from criminal background checks, though both represent important components of comprehensive healthcare screening programs. FACIS searches query federal exclusion databases to verify healthcare program participation eligibility, while criminal background checks examine court records to identify convictions and criminal history. Healthcare employers should conduct both FACIS screening and criminal background checks as these verification types address different risk dimensions.
Can healthcare organizations use automated services for FACIS screening or must searches be conducted manually?
Healthcare organizations may conduct FACIS screenings manually using free public database portals provided by the OIG and GSA, or utilize automated third-party screening services that query exclusion databases and provide ongoing monitoring with real-time alerts. Both approaches satisfy federal compliance requirements provided searches cover the LEIE and SAM.gov databases and occur with appropriate frequency. Automated monitoring systems typically reduce administrative burden and compliance risk by providing consistent coverage and immediate exclusion notifications.
How far back do FACIS exclusion records go?
The LEIE database maintained by the OIG includes all individuals and entities currently excluded from federal healthcare programs regardless of when the exclusion began, with records remaining in the database for the entire exclusion period. After exclusion periods expire and individuals obtain reinstatement, the OIG may archive exclusion records though historical exclusion information may remain accessible. Healthcare employers conducting FACIS screenings should focus on current exclusion status rather than historical records, as only active exclusions create program participation bars.
What information do healthcare employers need from candidates to conduct accurate FACIS screenings?
Healthcare employers should collect full legal names, dates of birth, and Social Security numbers to conduct accurate FACIS database searches that minimize false positive matches to individuals with similar identifying information. While the LEIE allows searches using name and state, incorporating additional identifiers improves matching accuracy. Healthcare employers must obtain proper written authorization from candidates before conducting background screenings, following Fair Credit Reporting Act requirements when using third-party consumer reporting agencies to perform verification services.
Do healthcare employers need to conduct FACIS checks on independent contractors and vendors?
Yes, healthcare organizations must verify that independent contractors, vendors, and any individuals or entities providing items or services billed to federal healthcare programs do not appear on exclusion lists. The OIG has emphasized that healthcare providers cannot circumvent exclusion screening requirements by using independent contractor relationships rather than direct employment arrangements. Healthcare compliance programs should extend FACIS screening and ongoing monitoring to all contractors and vendors involved in federal program service delivery.
Can individuals request removal from federal exclusion lists if they believe the exclusion was unjustified?
Excluded individuals may request reinstatement after exclusion periods expire by submitting formal reinstatement applications to the OIG that demonstrate factors leading to exclusion have been resolved. Reinstatement is not automatic; the OIG evaluates multiple factors including conduct during the exclusion period and whether debts related to the exclusion have been paid. Individuals who believe exclusion records contain factual errors may contact the OIG to request corrections, though substantive challenges to exclusion authority typically require administrative appeals filed within specified timeframes.
Additional Resources
- Office of Inspector General - List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/ - System for Award Management Exclusions
https://sam.gov/content/exclusions - Centers for Medicare & Medicaid Services - Screening Requirements
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-12.pdf - Federal Trade Commission - Fair Credit Reporting Act
https://www.ftc.gov/enforcement/statutes/fair-credit-reporting-act
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub

How Long Do Background Checks Take for Government Jobs? Timeline Expectations for 2026
6 Jan, 2026 • 20 min read
Driver Qualification File Requirements: Your Complete DOT Compliance Guide
6 Jan, 2026 • 18 min read
Healthcare Background Screening Costs: 2026 Budget Planning Guide for Medical Facilities
30 Dec, 2025 • 23 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.


