Healthcare employee background checks have evolved beyond single-point verifications to include continuous monitoring systems that track federal exclusion lists, state abuse registries, and licensing status throughout employment. Risk-stratified screening protocols now determine verification depth based on patient interaction levels, while emerging compliance challenges include navigating state-specific cannabis offense policies and verifying credentials for remote healthcare workers.
Key Takeaways
- Healthcare facilities must verify candidates against federal exclusion databases including the OIG LEIE and GSA SAM to maintain Medicare and Medicaid participation eligibility.
- Risk-stratified screening protocols adjust verification depth based on role requirements, with direct patient care positions requiring more extensive multi-state criminal checks than administrative roles.
- Continuous monitoring systems supplement traditional point-in-time verifications by providing ongoing alerts about license changes, exclusion list additions, and new criminal records.
- State-specific abuse registries, including child and adult protective services databases, require separate verification beyond federal checks for healthcare worker screening.
- Cannabis-related offense policies vary significantly by state, creating complex compliance considerations for healthcare employers in legalized jurisdictions.
- Remote healthcare worker verification introduces additional challenges for credential authentication, work location compliance, and multi-state licensing requirements.
- FACIS® database integration enables real-time checks against fraud and abuse records that may not immediately appear in traditional criminal background searches.
- Individualized assessments remain legally required even when disqualifying records appear, balancing patient safety concerns with fair hiring practices and state ban-the-box regulations.
Understanding Healthcare Employee Background Check Requirements
Healthcare employee background check processes differ substantially from general employment screening due to heightened patient safety concerns, vulnerable population protection mandates, and strict regulatory oversight. Healthcare facilities face consequences ranging from civil monetary penalties to loss of federal funding participation when screening failures allow excluded or prohibited individuals into patient care roles.
Federal regulations establish baseline requirements that apply across all states, while state licensing boards, health departments, and municipal ordinances layer additional mandates that vary by jurisdiction and facility type. Understanding this regulatory framework helps compliance officers build screening programs that satisfy all applicable requirements without creating unnecessary barriers to qualified candidates.
Federal Baseline Requirements for Healthcare Screening
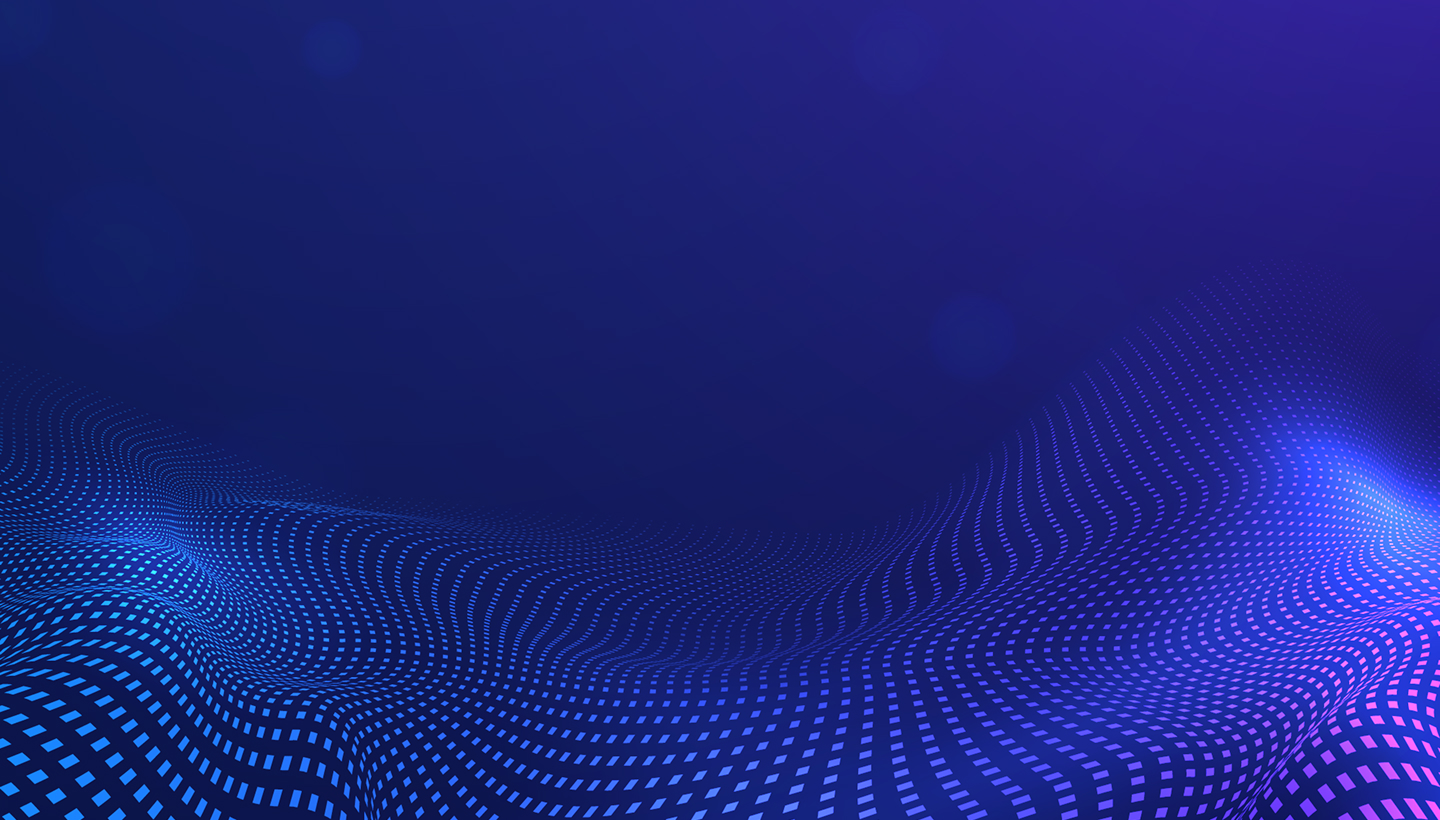
The federal government mandates specific healthcare worker screening requirements tied to Medicare and Medicaid participation. Facilities receiving federal healthcare funding must verify that employees, contractors, and vendors do not appear on exclusion lists maintained by the Office of Inspector General (OIG) or the General Services Administration (GSA). Key federal verification components include:
- OIG List of Excluded Individuals and Entities (LEIE): Contains healthcare providers and suppliers barred from federally funded programs due to fraud, patient abuse, licensing violations, or controlled substance convictions
- GSA System for Award Management (SAM): Identifies individuals and entities excluded from federal contracts and certain federal benefits
- Initial and ongoing verification: Required at hire and periodically throughout employment to detect new exclusions
- Vulnerable population requirements: Long-term care facilities participating in Medicare or Medicaid must conduct background checks consistent with state requirements under Patient Protection and Affordable Care Act provisions
While overlap exists between OIG and GSA databases, each contains unique entries, making verification against both systems necessary for comprehensive compliance.
State and Local Healthcare Screening Mandates
State requirements for healthcare employee background checks vary significantly in scope, methodology, and disqualifying criteria. Most states require criminal background checks for licensed healthcare professionals as a condition of initial licensure and renewal, with state licensing boards conducting these verifications directly or requiring proof of completion.
| Verification Component | Typical State Requirements | Common Variations |
| Criminal History Checks | Mandatory for direct care roles | Single-state vs. multi-state scope |
| Abuse Registry Searches | Required in most states for vulnerable populations | Child, adult, or both registries |
| Fingerprint-Based FBI Checks | Varies by state; some require for nursing homes/behavioral health | Requirements differ significantly by jurisdiction and facility type |
| Cannabis Offense Consideration | Varies by state legalization status | Some states prohibit employment decisions |
| Lookback Periods | 7–10 years common | Some states require full adult history |
State abuse registry requirements create additional verification obligations. Most states maintain central registries of substantiated abuse, neglect, or exploitation findings involving children, elderly individuals, or adults with disabilities. Healthcare workers in direct care roles typically require clearance from relevant state registries, though registry access procedures, search capabilities, and reporting consistency vary widely.
State cannabis legalization laws introduce complexity for healthcare employers conducting criminal background checks. Some states prohibit employment decisions based solely on cannabis possession convictions that are legal under current state law, while federal healthcare facilities and positions involving federal contracts face conflicting obligations due to continued federal prohibition. Employers should verify specific requirements in their jurisdiction and consult legal counsel regarding their particular circumstances.
Healthcare Facility Type and Accreditation Considerations
Different healthcare facility types face varying baseline requirements based on licensure categories and populations served. Hospitals, ambulatory surgical centers, skilled nursing facilities, intermediate care facilities, home health agencies, and behavioral health treatment programs each operate under distinct regulatory frameworks that may impose specific screening mandates.
Facilities serving vulnerable populations typically face enhanced screening requirements. Pediatric facilities, psychiatric hospitals, facilities for individuals with developmental disabilities, and substance abuse treatment centers often encounter stricter background check mandates due to patient vulnerability and historical abuse concerns.
Risk-Stratified Screening Protocols in Healthcare Settings
Healthcare employers increasingly implement tiered verification frameworks that adjust screening depth based on position-specific risk factors. This risk-stratified approach recognizes that different roles present varying levels of patient safety concerns, access to controlled substances, handling of sensitive information, and vulnerability exposure.
| Position Category | Patient Interaction | Typical Screening Components |
| Direct Care Providers | High, hands-on treatment | Multi-state criminal, federal exclusion, abuse registries, license verification, education confirmation, possible FBI fingerprint |
| Indirect Patient Contact | Moderate, limited interaction | Criminal background, exclusion verification, potentially narrower geographic scope |
| Administrative/Support | Minimal or none | Baseline criminal check, exclusion verification, role-specific risk assessment |
Direct patient care providers, including nurses, physicians, therapists, and patient care technicians, typically undergo the most comprehensive screening due to hands-on patient interaction, medication access, and vulnerable population contact. Administrative and support staff with minimal or no patient interaction often undergo baseline criminal background checks and exclusion verification but may not require abuse registry searches or multi-state criminal history verification unless role-specific risk factors warrant expanded screening.
Components of Comprehensive Healthcare Background Checks
Criminal History Verification
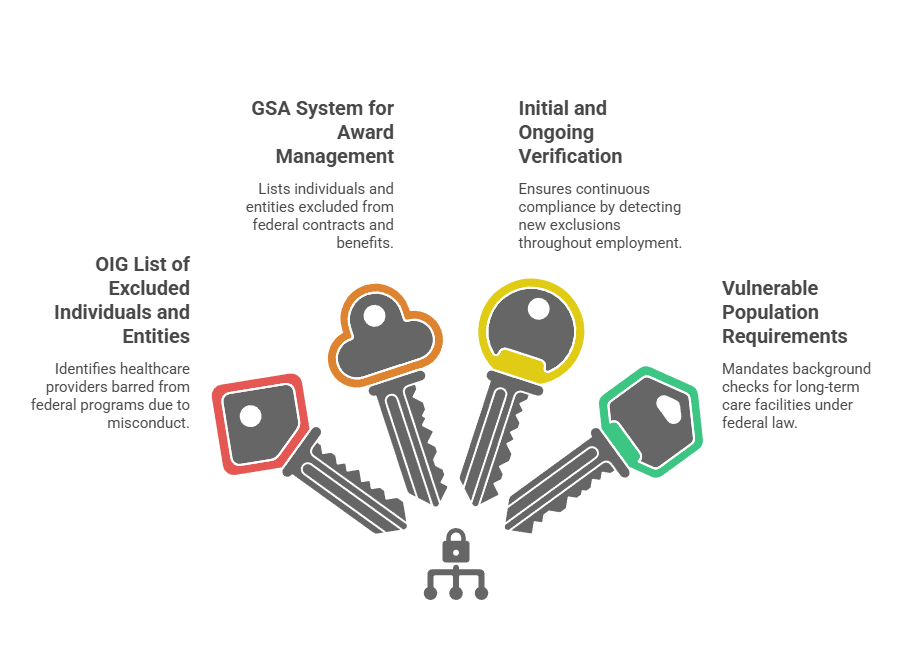
Criminal history checks form the foundation of healthcare background screening. These searches help identify convictions or pending cases that may pose patient safety, compliance, or operational risk. Common criminal history components include:
- County-level criminal court searches
These searches return detailed felony and misdemeanor records from specific jurisdictions where a candidate has lived, worked, or studied. - State criminal database searches
State databases provide broader geographic coverage but may contain delayed updates or limited case details. Results often require follow-up verification. - Federal criminal searches
Federal court searches identify offenses prosecuted at the federal level, including healthcare fraud, controlled substance violations, and crimes committed on federal property. - Sex offender registry searches
These searches verify whether a candidate appears on state or national sex offender registries.
Multi-state criminal searches are often necessary in healthcare. Many workers relocate for education, training, or employment, which creates screening obligations across multiple jurisdictions.
Federal Exclusion and Sanctions Screening
Federal exclusion screening is a required component for healthcare organizations that bill federal programs. Employers must verify candidates against exclusion lists before hire and throughout employment. Required sources include the OIG List of Excluded Individuals and Entities (LEIE) and the GSA System for Award Management (SAM).
These databases identify individuals barred from participation in federally funded healthcare programs or government contracts. Employing an excluded individual can create immediate liability, even if the employer was unaware of the exclusion at the time of hire. Because exclusions can occur after onboarding, ongoing monitoring is necessary to maintain compliance.
FACIS® Database Searches
FACIS® searches add an additional layer of risk visibility beyond traditional criminal and exclusion checks. The FACIS database aggregates fraud, abuse, and sanction records from multiple federal and state sources. FACIS® may include:
- Medicare and Medicaid exclusions
- License revocations and restrictions
- Controlled substance violations
- Healthcare-related criminal convictions
- Civil judgments tied to healthcare fraud or abuse
Some FACIS records may not appear immediately in standard criminal databases. For this reason, FACIS® screening is often used alongside OIG and GSA checks to support more comprehensive healthcare risk assessments.
State Abuse Registry Searches
Most states maintain registries of substantiated abuse, neglect, or exploitation involving vulnerable populations. These registries operate separately from criminal courts and require additional clearance steps. Healthcare employers may need to search:
- Child abuse registries
- Adult protective services registries
- Healthcare worker misconduct registries
Access methods vary by state. Some registries allow online searches, while others require fingerprint submissions or formal requests. Each registry serves a different purpose and may require a separate search.
Professional License Verification
License verification confirms that healthcare professionals hold active and unrestricted credentials. This process relies on primary source verification with state licensing boards. Verification typically confirms:
- License number and type
- Issue and expiration dates
- Current license status
- Disciplinary actions or practice restrictions
License status can change during employment. Ongoing monitoring helps employers identify suspensions, expirations, or disciplinary actions that affect eligibility to practice.
Sex Offender Registry Considerations
Sex offender registry findings raise serious patient safety concerns, especially in pediatric or vulnerable population settings. However, automatic disqualification policies may not be permitted in all jurisdictions.
Employers should conduct individualized assessments that consider:
- The nature of the offense
- Time elapsed since the incident
- Evidence of rehabilitation
- The duties and risk profile of the role
This approach supports patient protection while aligning with fair hiring requirements.
Navigating Complex Compliance Requirements
Healthcare employers must navigate overlapping and sometimes conflicting requirements from federal regulations, state laws, municipal ordinances, licensing board rules, and facility-specific policies. Compliance challenges arise when these requirements diverge or when applying general employment laws to healthcare-specific screening scenarios.
Federal and State Law Intersection Points
Ban-the-box laws in numerous states and municipalities restrict when employers may inquire about criminal history or how criminal records influence employment decisions. Some jurisdictions prohibit criminal history questions on initial applications, require individualized assessments before adverse action based on criminal records, or limit consideration to convictions rather than arrests.
The Fair Credit Reporting Act (FCRA) governs how employers obtain and use background check information from consumer reporting agencies. FCRA compliance requires clear written disclosure in a standalone document, separate candidate authorization, pre-adverse action procedures including provision of the consumer report and Summary of Rights with reasonable time for candidate response, and final adverse action notices.
Equal Employment Opportunity Commission (EEOC) guidance addresses the use of criminal background information in employment decisions. The EEOC position emphasizes individualized assessment considering offense nature, time elapsed, and job relevance rather than blanket disqualification policies.
Multi-State Workforce and Remote Work Complications
Healthcare workforce mobility creates verification challenges when candidates have lived, worked, or been educated across numerous states. Comprehensive screening requires identifying all relevant jurisdictions, understanding state-specific records access procedures, and managing varying processing timeframes across different court systems and government agencies.
Remote healthcare workers, including telemedicine providers, remote patient monitoring staff, and administrative personnel, introduce additional complexity:
- May require licensure in multiple states where patients are located
- Trigger background check requirements in each practice jurisdiction
- Necessitate ongoing monitoring of multi-state regulatory compliance
- Create questions about which state's employment laws and screening requirements apply
Determining which state's employment laws and screening requirements apply to remote workers involves complex analysis of factors including employee residence, employer location, and service delivery locations. Healthcare employers should consult legal counsel to assess applicable requirements for remote worker arrangements in their specific circumstances.
Traveling healthcare professionals, such as temporary nurses or locum tenens physicians, present recurring verification challenges. Some facilities require full background checks for each new assignment, while others accept recent verifications from previous assignments or credentials verification organizations.
Managing Disqualifying Information and Individualized Assessments
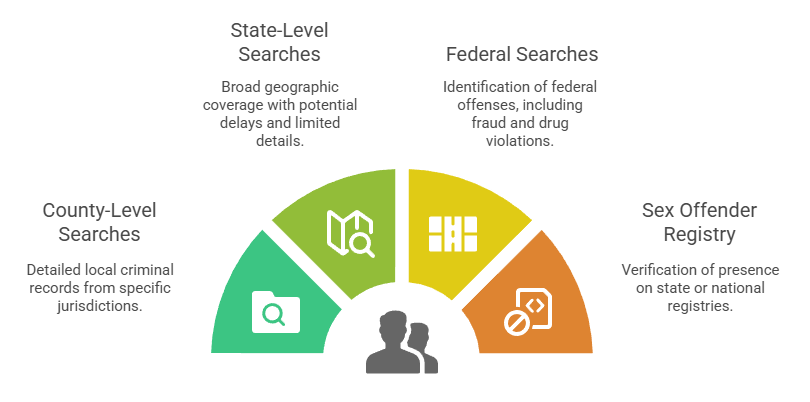
When background checks reveal potentially disqualifying information, healthcare employers face decisions balancing patient safety, regulatory compliance, fair hiring practices, and legal risk. Automatic disqualification policies without individualized consideration create legal vulnerability under EEOC guidance and some state laws.
Individualized assessments should consider:
- Offense nature and gravity: Severity and relevance to patient care responsibilities
- Time elapsed: Period since offense or sentence completion
- Position nature: Specific job duties and patient interaction level
- Rehabilitation evidence: Subsequent education, training, character references, or certificates of rehabilitation
Candidates must receive opportunity to provide context, evidence of rehabilitation, or information demonstrating that records are inaccurate or incomplete. Facilities should establish procedures for candidates to submit additional information and timelines for consideration.
State healthcare employment laws may limit individualized assessment discretion by mandating disqualification for specific offense types or creating statutory bars subject only to formal waiver or exemption processes.
Record Accuracy and Dispute Resolution
Background check records sometimes contain errors, omissions, or outdated information that can unfairly impact candidates. Common issues include mismatched identity where records belong to different individuals with similar names, incomplete disposition information showing arrests without subsequent case outcomes, sealed or expunged records that should not appear in background reports, and outdated information reflecting superseded court actions or corrected data.
Candidates have rights to dispute inaccurate background check information under the FCRA and similar state laws. Employers using consumer reporting agencies for background checks must provide dispute procedures and allow reasonable time for investigation before finalizing adverse decisions. Consumer reporting agencies must reinvestigate disputed information, typically within 30 days, and correct or remove information that cannot be verified.
Continuous Monitoring and Ongoing Compliance
Initial background checks provide point-in-time verification, but healthcare worker compliance status changes throughout employment due to new criminal charges, license discipline, exclusion list additions, or registry entries. Facilities must implement ongoing monitoring strategies to maintain continuous compliance rather than relying solely on hire-date verification.
Periodic Re-Screening Requirements
Many states and federal programs mandate periodic background check updates at specified intervals. For example, some states require nursing home employee re-screening every two to five years. Medicare enrollment regulations require monthly verification against federal exclusion lists, though many facilities conduct this verification more frequently.
| Monitoring Component | Typical Frequency | Regulatory Basis |
| Federal Exclusion Lists | Monthly minimum | CMS requirements |
| Professional License Status | Quarterly to annual | State licensing board rules |
| Criminal History Updates | Every 2–5 years | State facility licensing requirements |
| Abuse Registry Checks | Every 2–5 years | State vulnerable population protection laws |
Triggering events may warrant immediate re-screening outside regular intervals, following applicable procedural requirements including disclosure and authorization. These may include substantiated allegations of misconduct, patient safety incidents, criminal convictions where legally permissible to consider, license discipline notifications, or documented performance issues. Employers should verify that re-screening policies comply with state laws regarding consideration of arrests versus convictions and procedural protections for current employees.
Automated Monitoring Systems
Technology-enabled continuous monitoring supplements periodic manual re-screening by automatically tracking relevant databases and generating alerts when new adverse information appears. These systems typically monitor federal exclusion lists for monthly additions, state licensing boards for disciplinary actions or status changes, criminal record databases for new charges or convictions, and in some cases, sex offender registries and abuse registries for new entries.
Automated monitoring reduces compliance gaps between periodic re-screening intervals and decreases administrative burden compared to manual monthly exclusion list verification. Alert triage procedures determine how facilities respond when monitoring systems generate notifications.
Managing Exclusions and Disqualifying Events During Employment
When current employees appear on exclusion lists, receive disqualifying convictions, or experience other events that would have prevented initial hire, facilities face difficult decisions regarding continued employment. Federal exclusion list additions create strict liability exposure for continued Medicare or Medicaid billing related to the excluded individual's services, typically requiring immediate separation or reassignment to non-federally funded roles.
License suspensions or revocations may prevent licensed professionals from practicing during discipline periods, requiring temporary reassignment, leave of absence, or separation depending on circumstances and duration.
Practical Implementation Strategies for Healthcare Employers

Building effective healthcare background screening programs requires translating regulatory requirements into operational procedures that ensure compliance while supporting hiring objectives and workforce needs.
Developing Position-Specific Screening Protocols
Healthcare organizations should conduct position-by-position risk assessments that identify specific verification requirements for each role:
- Patient contact level and vulnerability exposure
- Medication and controlled substance access
- Sensitive information handling responsibilities
- Regulatory requirements specific to the role
- Potential harm scenarios relevant to job duties
Documentation of risk assessment rationale supports defensible screening decisions and demonstrates thoughtful compliance approaches if policies face scrutiny.
Candidate Communication and Transparency
Clear communication with candidates about background check processes, timeframes, and implications helps set appropriate expectations and reduces friction during screening. Pre-application or early-application disclosure of background check requirements, general disqualification criteria, and candidate rights promotes transparency and allows self-selection by candidates with known disqualifying issues.
Consent and authorization forms should clearly explain what information will be obtained, how it will be used, and candidate rights under applicable laws. FCRA-compliant disclosure and authorization requires specific formatting, language, and separation from other documents.
Balancing Thoroughness with Hiring Timeline Pressures
Healthcare staffing shortages create pressure to accelerate hiring processes, sometimes conflicting with comprehensive background screening timelines. Criminal background checks from some jurisdictions, abuse registry searches in certain states, and international education verification can require weeks or longer for completion.
Conditional employment offers pending final background check clearance, issued after proper FCRA disclosure and authorization, allow onboarding processes to begin while verification continues. Direct patient care typically cannot begin until full clearance, and any offer revocation based on background check results must follow complete adverse action procedures including candidate notification and opportunity to respond.
Restricted duty assignments, supervised orientation periods, or administrative responsibilities may bridge gaps between hiring and final clearance for some roles.
Vendor Management and Quality Assurance
Healthcare employers using consumer reporting agencies or background screening vendors must verify that providers understand healthcare-specific requirements, maintain appropriate database access and court researcher networks, comply with FCRA and state consumer reporting laws, and deliver accurate, timely results.
Service agreements should specify:
- Exact verification components and geographic coverage
- Search methodology and court researcher networks
- Turnaround time commitments and expedite procedures
- Accuracy standards and error resolution procedures
- Data security and privacy protections
- Compliance responsibilities and audit rights
Quality assurance processes verify background check accuracy and completeness through periodic result audits, vendor performance monitoring, candidate feedback mechanisms, and comparison of similar searches across different vendors or time periods.
Documentation and Recordkeeping
Comprehensive documentation supports compliance verification during audits, defends against discrimination claims, and demonstrates good-faith reasonable care in hiring. Background check files should include authorization forms and disclosures, complete verification reports, adverse action notices if applicable, individualized assessment documentation, and candidate response documentation.
Data security and confidentiality protections for background check records must meet applicable privacy law requirements including FCRA disposal rules, state data breach notification laws, and industry standards. Sensitive information including Social Security numbers, dates of birth, criminal records, and medical information requires secure storage with restricted access controls and proper disposal procedures such as shredding or electronic data destruction. Employers should verify specific requirements applicable to their jurisdiction and industry sector.
Conclusion
Healthcare employee background checks require navigating complex regulatory frameworks, implementing risk-appropriate verification protocols, and maintaining ongoing monitoring to protect patients and ensure compliance. Effective programs balance thoroughness with operational realities while respecting candidate rights and legal requirements.
Frequently Asked Questions
What background checks do hospitals require for new employees?
Hospitals typically require criminal background checks, federal exclusion list verification (OIG and GSA), state abuse registry clearances, professional license verification for licensed staff, and education confirmation. Specific requirements vary based on position type, state regulations, and facility policies.
How far back do healthcare background checks go?
Healthcare background check lookback periods vary by state law, record type, and facility policy. Criminal history searches commonly cover seven to ten years, though some states require or permit longer periods for healthcare positions. Federal exclusion lists and professional license discipline have no time limits.
Can healthcare workers with criminal records get hired?
Healthcare employment with criminal records depends on offense type, time elapsed, position requirements, state regulations, and individualized circumstances. Many states mandate disqualification for specific convictions including patient abuse, violent crimes, or healthcare fraud. Other offenses may allow employment after individualized assessment considering rehabilitation, job relevance, and risk factors.
What is continuous monitoring for healthcare employees?
Continuous monitoring involves automated tracking of databases including federal exclusion lists, criminal records, professional licenses, and abuse registries throughout employment rather than only at hire. Systems generate alerts when new adverse information appears, enabling facilities to maintain ongoing compliance between periodic re-screening intervals.
Do healthcare employers check all states where I have lived?
Comprehensive healthcare background checks typically include criminal searches in states where candidates have lived, worked, or attended school during relevant lookback periods. Some facilities limit searches to current residence and recent prior locations, while others conduct nationwide database searches supplemented by county-level checks in identified jurisdictions.
What happens if my background check contains errors?
Candidates have rights to dispute inaccurate background check information under the Fair Credit Reporting Act and similar state laws. Employers must provide procedures for challenging records and allow reasonable time for investigation before finalizing adverse decisions. Consumer reporting agencies must reinvestigate disputed information within 30 days and correct or remove unverifiable records.
Are cannabis convictions disqualifying for healthcare jobs?
Cannabis offense impact on healthcare employment varies by state law, facility type, and position requirements. Some states prohibit employment decisions based solely on cannabis possession convictions that are legal under current state law, while federal healthcare facilities and roles involving federal contracts face conflicting obligations due to continued federal prohibition. Employers should verify specific requirements in their jurisdiction and consult legal counsel regarding their particular circumstances.
How long does a healthcare background check take?
Healthcare background check completion typically requires one to three weeks, though complex verifications involving multiple states, international education, or slow-responding agencies may take longer. Incomplete candidate information, common name matching issues, or record discrepancies requiring additional research also affect processing times.
Additional Resources
- Office of Inspector General List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/ - System for Award Management (SAM) Exclusions
https://sam.gov/content/exclusions - Centers for Medicare & Medicaid Services Background Check Resources
https://www.cms.gov/ - U.S. Equal Employment Opportunity Commission Background Checks Guidance
https://www.eeoc.gov/laws/guidance/enforcement-guidance-consideration-arrest-and-conviction-records-employment - Federal Trade Commission Fair Credit Reporting Act Resources
https://www.ftc.gov/legal-library/browse/statutes/fair-credit-reporting-act - National Practitioner Data Bank
https://www.npdb.hrsa.gov/

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.