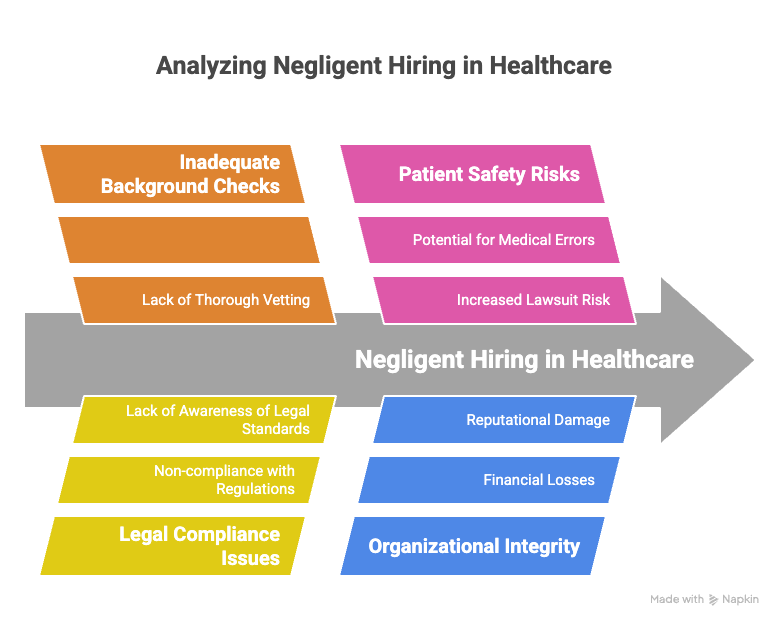
In the high-stakes world of healthcare, the hiring of unqualified or dangerous staff can lead to dire consequences. Healthcare negligent hiring not only jeopardizes patient safety but also exposes organizations to severe liability risks. Skipping comprehensive background checks poses significant challenges for healthcare providers, from facing costly lawsuits to endangering both reputation and safety.
This comprehensive guide explores the implications of healthcare negligent hiring, shedding light on its potential legal repercussions and offering best practices for mitigating these risks. Whether you are an HR professional in a hospital, clinic administrator, or healthcare executive, understanding negligent hiring is vital to safeguarding your organization.
Key Takeaways
- Negligent hiring in healthcare can lead to costly lawsuits and damage to a facility's reputation if staff harm patients due to inadequate background checks.
- Properly vetting medical staff through background checks is crucial to ensure patient safety and adhere to legal standards.
- Criminal history, professional licensure, employment history, and references are key elements of an effective background check process.
- Continuous monitoring of staff credentials and criminal records helps maintain compliance and protect patient safety.
- Familiarizing yourself with legal guidelines, such as the Fair Credit Reporting Act, ensures your hiring practices meet regulatory requirements and protect your organization.
Introduction
Imagine the fallout when a hospital hires a nurse with a history of malpractice who harms a patient. Unfortunately, these scenarios are not rare. In 2022, negligence lawsuits in healthcare hit a new high, with many tracing back to unvetted hires. Negligent hiring occurs when healthcare facilities bring in staff without proper background checks, risking patient lives and opening the door to legal battles. Itâs a costly gamble that threatens reputations and financial stability.
This article dives into the liabilities of skipping background checks in the healthcare sector. We'll explore the dangers involved and outline measures to minimize these risks effectively. Whether you manage a clinic's HR department or oversee a hospital's operations, grasping the impact of negligent hiring is essential for protection against avoidable pitfalls.
Understanding Healthcare Negligent Hiring
Negligent hiring in healthcare occurs when employers fail to thoroughly vet a candidate's background, resulting in hiring someone who could harm patients or pose a risk to the organization. It's more common than many realize. Research shows that lapses in background checks can lead to unqualified or even dangerous individuals gaining positions of trust. This compromises patient safety, wastes resources, and exposes organizations to costly legal battles.
Patient safety is at the heart of healthcare. A single oversight in hiring can lead to severe patient harm, triggering lawsuits. For instance, if an unvetted nurse administers incorrect medication, the hospital could face medical malpractice or wrongful death suits. These situations highlight the necessity of careful hiring practices.
On the legal front, employers need to be aware of the regulations surrounding negligent hiring. Various legal precedents establish that healthcare institutions can be held liable for the actions of their staff if it can be shown they did not conduct reasonable background checks. The U.S. Department of Labor provides guidelines on what is considered reasonable, offering a framework to ensure compliance and minimize risk.
Knowledge is power. Familiarize yourself with resources like the U.S. Department of Labor's site to understand legal obligations better. This will help you navigate the complex terrain of healthcare hiring while protecting both your patients and your organizationâs integrity.
Key Components of Medical Staff Background Checks
A thorough background check for medical staff is essential in maintaining a safe and reputable healthcare environment. This process consists of several key components that help ensure the right candidates are selected for crucial roles in patient care.
Criminal History
One of the primary steps in a background check is reviewing an applicant's criminal records. This is crucial in weeding out individuals who might pose a threat to patients or colleagues. Imagine the implications of hiring someone with a history of violence or theft. Not only does it jeopardize patient safety, but it also puts the entire organization at risk of legal repercussions. Make sure you access both federal and state databases for comprehensive results.
Professional Licensure
Verifying professional licenses is non-negotiable. In healthcare, credentials matter. An unlicensed nurse or doctor is a liability waiting to happen. Confirm that applicants hold valid and current licenses for their specializations. This can be done through state licensing boards or professional regulatory agencies. Even a minor oversight here can lead to disastrous patient outcomes and legal challenges.
Employment History
Reviewing past employment helps identify consistent patterns in behavior and performance. Look for unexplained gaps or frequent job changes, which may indicate problematic conduct. Contact previous employers to verify tenure, responsibilities, and reasons for leaving. This step can reveal red flags that a resume alone might not.
Reference Checks
Obtaining personal and professional references offers insight into a candidateâs work ethic and character. Ask references specific questions about the candidate's past performance, teamwork, and ethics. This can help you gauge whether they would be a good fit for your team. Emails and phone calls to previous supervisors often provide valuable feedback.
Continuous Monitoring
Conducting a one-time check is not enough. Set up systems for continuous monitoring to catch any new issues that might arise after hiring. This ongoing vigilance ensures that your staff remains qualified and compliant with regulatory standards. Consider using services that alert you to any changes in an employee's criminal status or licensure.
By focusing on these components, you better protect your patients, staff, and organization. Each step adds a layer of security and trust, crucial in the sensitive field of healthcare. Are you equipped to make these checks a standard part of your hiring process?
Potential Liability from Negligent Hiring in Healthcare
Skipping background checks in healthcare can lead to dire legal outcomes. Patient safety lawsuits top the list of potential liability risks. Imagine a scenario where a healthcare worker's negligence harms a patient. The legal repercussions could involve hefty settlements and lengthy court battles. These lawsuits not only drain finances but also tarnish reputations.
The damage to an organization's standing is another significant risk. When a healthcare provider is linked to negligent hiring, public trust takes a hit. Patients lose confidence in an institution riddled with such missteps. This loss of trust can lead to decreased patient retention and a decline in new patient acquisitions, affecting the bottom line.
Regulatory penalties are also a burden. Failing to perform proper background checks may result in fines from regulatory bodies. Non-compliance with hiring guidelines can attract penalties that strain financial resources. Moreover, rectifying compliance failures often requires additional training and oversight, contributing to the overall cost.
Financial consequences extend beyond lawsuits and penalties. The cost of legal defenses, settlements, and elevated insurance premiums can quickly mount. Staff turnover, another consequence, incurs costs in training and onboarding new hires to replace those implicated in questionable hiring practices.
In healthcare, diligent hiring is not just a best practice but a necessity. By ignoring proper background checks, healthcare organizations expose themselves to preventable liabilities. Is overlooking thorough vetting worth risking patient safety and organizational integrity?
Best Practices for Minimizing Healthcare Hiring Negligence
Implementing a thorough background check process is essential in reducing risks associated with negligent hiring. Start with criminal history checks to filter out individuals with potentially dangerous backgrounds. Verify all professional licenses and credentials to ensure candidates are qualified for their roles. Don't skip employment history reviews; these can reveal patterns of behavior that might pose risks.
References are crucial, too. Speak directly with past supervisors to get candid insights into the applicantâs work ethic and reliability. Make continuous monitoring a part of your strategy. Regular updates on staff credentials and criminal records help maintain a safe work environment and prevent compliance issues.
Stay compliant with legal standards like the Fair Credit Reporting Act (FCRA). Itâs important to inform candidates of any background checks and secure their consent. Training your HR staff on these procedures ensures everyone understands legal requirements and best practices.
Keep records of every step in your hiring process. Documenting background checks, decisions, and HR procedures can protect your organization in potential legal disputes. Regularly update these policies to keep up with the latest regulations and industry practices.
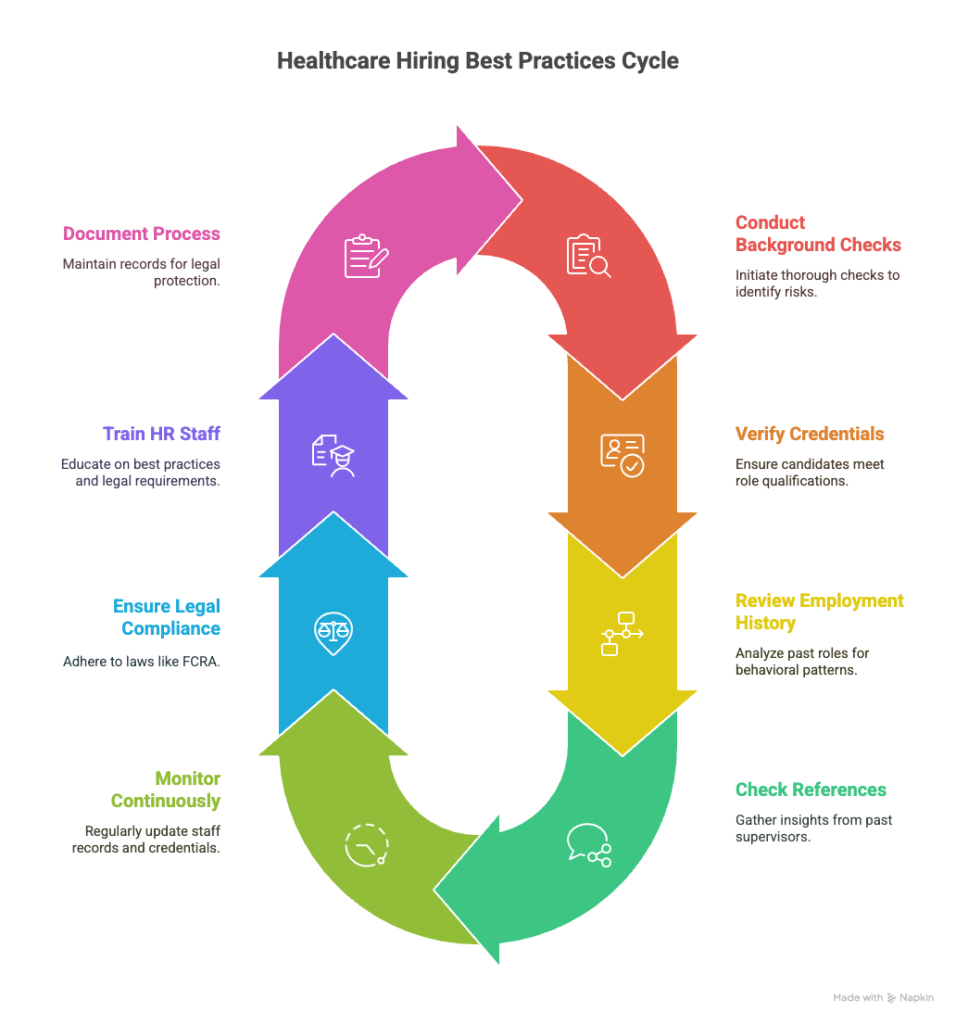
Adopting these strategies not only minimizes risks but also secures your healthcare organizationâs reputation and operational integrity.
Healthcare Compliance Risks and the Role of FCRA
The Fair Credit Reporting Act (FCRA) serves as a crucial framework for healthcare hiring by governing how organizations can use consumer reports, including background checks. You must ensure that every step of your hiring process aligns with the FCRA to avoid legal issues and hefty penalties. Compliance is non-negotiable and essential to maintaining the integrity of your hiring practices.
To navigate FCRA compliance, begin by obtaining written consent from job applicants before conducting background checks. This is a legal requirement and a fundamental aspect of respecting candidate privacy. If you decide not to hire someone based on their background check, provide them with a pre-adverse action notice. Include a copy of the report and a summary of their rights under the FCRA. If you proceed with the adverse action, follow up with a post-adverse action notice. This transparency is not only a legal obligation but also a sign of professional courtesy.
Common pitfalls in FCRA compliance often stem from neglecting these formalities. Some healthcare organizations fail to properly notify applicants, risking legal penalties. Mitigating these risks involves regular training for HR staff on FCRA requirements and frequent audits of your hiring processes.
Ask yourself: Are your hiring practices fully aligned with FCRA regulations? Regular assessments can ensure compliance and protect your organization from unnecessary legal challenges. By embedding these practices into your hiring strategies, you safeguard your organization and promote a culture of compliance and transparency.
Conclusion
Skipping healthcare background checks can lead to serious liability risks and jeopardize patient safety. When organizations bypass these critical steps, they open the door to hiring unqualified or potentially dangerous individuals. The consequences can include costly lawsuits, regulatory penalties, and a damaged reputation.
One key point is that healthcare providers might face patient safety lawsuits if negligent hiring results in harm. These legal battles are not only expensive but may also tarnish an organization's name, leading to a loss of trust among patients and staff. Regulatory bodies may impose fines for non-compliance with hiring laws, further increasing financial strain.
Beyond legal and monetary setbacks, the reputation damage from negligent hiring can be severe. Trust takes years to build and moments to destroy. Patients rely on healthcare institutions for safe and competent care. A single incident can lead to long-term reputational harm.
Focusing on diligent hiring practices offers substantial benefits. Conducting thorough background checks can prevent these risks and enhance patient safety. It also reflects a commitment to excellence and responsibility, vital for maintaining a respected position in the healthcare community.
Healthcare organizations should prioritize robust protocols in their hiring process. Stay vigilant, keep current with regulations, and maintain the integrity of your institution. Robust background checks are an investment, not just a compliance task, in fostering a safe and reliable healthcare environment.
Frequently Asked Questions (FAQs)
What are the risks of not doing background checks in healthcare?
Without background checks, healthcare organizations risk hiring individuals with criminal records, false credentials, or past employment issues. This can lead to compromised patient care, legal troubles, and reputational damage.
Can a hospital be sued for negligent hiring?
Yes, a hospital can face lawsuits for negligent hiring if an employee causes harm due to a lack of proper background screening. The organization may be held liable for damages resulting from the employeeâs actions.
Are background checks required by law in healthcare?
Background checks are mandated by law for certain healthcare positions. The requirements can vary by state and specific role, so it's important to understand local regulations and ensure compliance.
What background checks are legally necessary for nurses and doctors?
For nurses and doctors, checks often include criminal history, professional license verification, education verification, and employment history. Drug screening may also be required, depending on the state's laws.
What is the liability for hiring an excluded individual?
Hiring an excluded individual can lead to severe penalties, including fines and loss of federal funding. Healthcare providers must ensure that potential employees are not on the exclusion list.
What types of criminal records are typically examined in healthcare background checks?
Healthcare background checks usually review records related to violent crimes, theft, fraud, and other offenses that could impact patient safety and trust.
How long do background checks usually take in the healthcare industry?
Background checks in healthcare typically take anywhere from a few days to a couple of weeks, depending on the depth of the check and the response time of various checking agencies.
Can previous employment gaps affect hiring in healthcare?
Yes, employment gaps may be scrutinized during the hiring process. It is crucial to provide honest and clear explanations for any gaps to avoid potential issues.
What happens if discrepancies are found during a background check?
If discrepancies are found, employers can request clarification from the candidate. Consistent discrepancies might result in the withdrawal of a job offer.
Definitions
Negligent Hiring
Negligent hiring happens when an employer fails to check a candidateâs background thoroughly, leading to the employment of someone who poses a safety or legal risk. In healthcare, this could mean hiring a nurse with a history of malpractice without verifying credentials. If that person harms a patient, the employer could be held responsible for damages.
Background Check
A background check reviews a candidateâs history, such as criminal records, employment, and education, to assess whether they're fit for a role. In healthcare, this step protects patients and ensures compliance with laws. Skipping it can result in lawsuits or harm to your organizationâs reputation.
Professional Licensure
Professional licensure is proof that a healthcare worker is qualified and authorized to perform specific duties. Itâs issued by state boards or regulatory agencies. Hiring someone without a valid license can lead to legal consequences and patient safety risks. Always confirm that licenses are current.
Reference Check
A reference check involves contacting former supervisors or colleagues to learn more about a candidateâs job performance and character. This adds context beyond resumes and interviews. For example, someone might look great on paper but have a record of poor teamwork or misconduct. Speaking with former employers helps you catch warning signs early.
Fair Credit Reporting Act (FCRA)
The FCRA is a federal law that governs how employers use consumer reports, including background checks. You must get written permission from candidates before checking their records. If you decide not to hire based on the report, you need to follow specific notices. Failing to follow FCRA rules can lead to lawsuits or fines. Are your hiring practices aligned with this law?
References
- Envoyâs negligent hiring case study:
https://www.envoy.us/post/we-reviewed-1350-negligent-hiring-cases-and-settlements-and-here-s-what-we-found - Legal Action Centerâs Second Chance Employment Report:
https://www.lac.org/assets/files/Second-Chance-Employment-Report.pdf - CoverLink nuclear verdict case study:
https://coverlink.com/case-study/nuclear-verdict-case-study-7-34-billion-negligent-hiring-retention-supervision-loss/

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.