Home health aide background check requirements combine federal Medicare/Medicaid mandates with state-specific regulations that vary significantly across jurisdictions, creating complex compliance obligations for agencies. This comprehensive guide addresses the critical screening requirements, disqualifying offenses, turnaround timelines, and risk mitigation strategies that home healthcare administrators must implement to maintain regulatory compliance and protect vulnerable populations.
Key Takeaways
- Federal law requires all Medicare/Medicaid-certified home health agencies to conduct comprehensive background checks including FBI fingerprinting, state criminal history, and abuse registry searches before hiring aides.
- The 21st Century Cures Act mandates nationwide criminal background checks for long-term care workers, with most states requiring both state and federal-level screening.
- Disqualifying offenses typically include violent crimes, sexual offenses, abuse/neglect convictions, and theft-related crimes, though lookback periods range from 5 years to lifetime depending on offense severity and state law.
- State-specific requirements create a patchwork of compliance obligations, with some states mandating additional screenings like child abuse registries, drug testing, and tuberculosis screenings beyond federal minimums.
- Background check turnaround times average 3-14 business days, though FBI fingerprint processing can extend timelines and impact your agency's ability to onboard qualified candidates quickly.
- Non-compliance penalties include Medicare/Medicaid decertification, civil fines up to $10,000 per violation, and increased liability exposure in negligent hiring lawsuits.
- Conditional hiring practices allow agencies to begin training while awaiting background check results, but direct patient contact must be prohibited until clearance is obtained.
- Annual recertification requirements exist in 23 states, requiring ongoing monitoring systems rather than one-time screening at hire.
Federal Background Check Requirements for Home Health Aides
The foundation of home health aide background check requirements stems from federal regulations that apply to all agencies receiving Medicare or Medicaid reimbursement. Understanding these baseline requirements is essential before navigating state-specific additions. The Centers for Medicare & Medicaid Services (CMS) establishes strict standards that create the compliance floor for all home healthcare providers.
Medicare and Medicaid Mandated Screenings
CMS requires home health agencies to comply with Section 6201 of the Affordable Care Act, which established national background check standards for long-term care workers. These requirements apply to all Medicare/Medicaid-certified agencies regardless of size or patient volume. The regulations mandate specific screening components completed before any direct patient care begins.
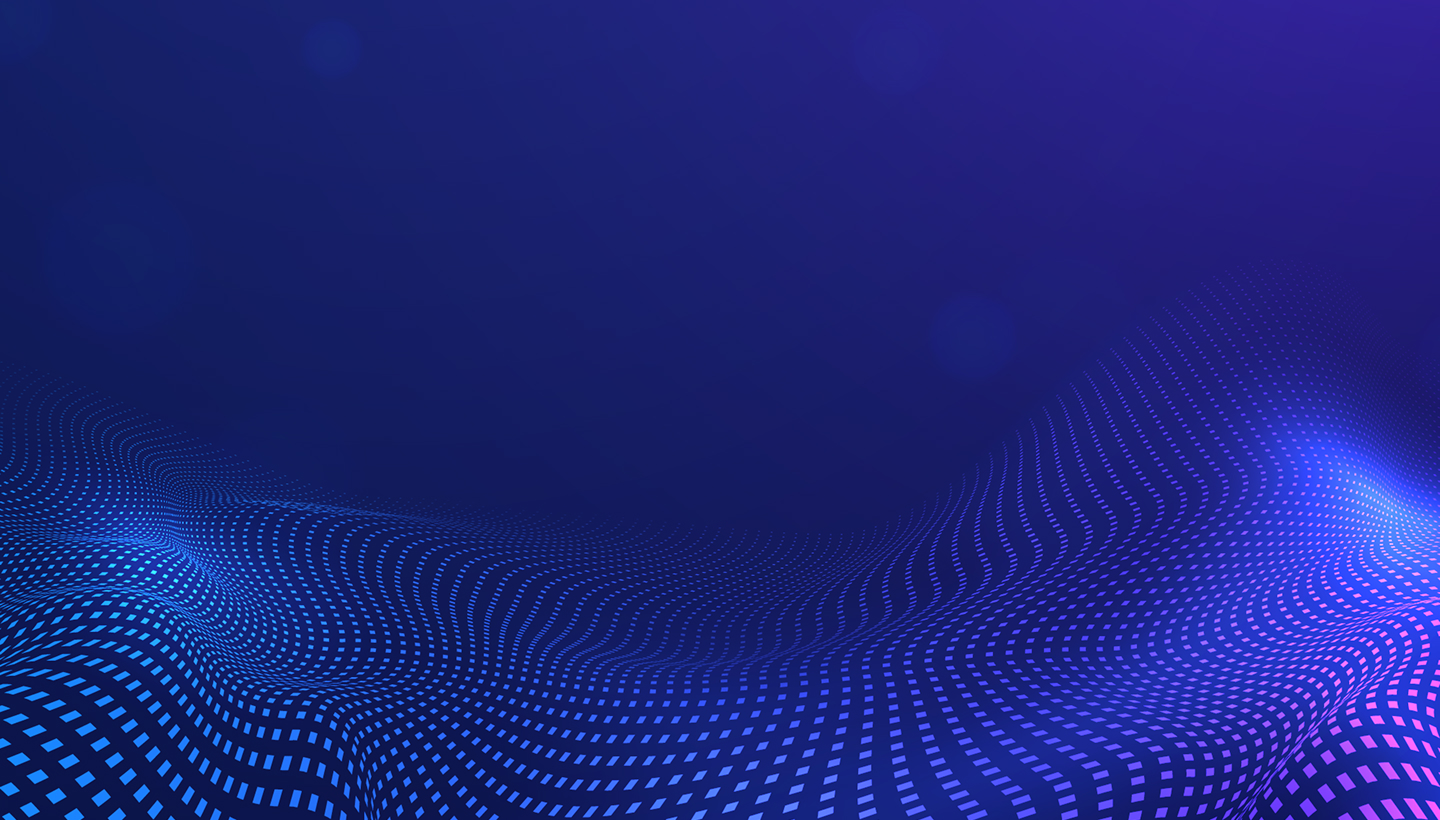
All agencies must conduct the following screenings:
- State criminal history repository checks: Cover felony and misdemeanor convictions in states where the applicant resided.
- National Sex Offender Public Website searches: Include all states where the candidate has lived or worked.
- Abuse and neglect registry checks: Must verify in every state where the applicant previously provided care services.
- FBI fingerprint-based criminal background checks: Required when mandated by individual state law.
The 42 CFR §424.530 regulation specifically prohibits agencies from employing individuals with disqualifying criminal convictions. This creates strict liability standards where non-compliance can result in immediate Medicare decertification.
My experience working at organizations that deal with roles involving the care of others has made me realize that recruitment has a long-term impact even after the recruitment process is complete. The process of doing background checks is not just about completing an added requirement; it’s actually about upholding the trust reposed in organizations and institutions. The aftermath of an improper recruitment process sometimes manifests silently and painfully later on.
The 21st Century Cures Act Impact
Enacted in 2016, the 21st Century Cures Act strengthened background check requirements significantly. The Act mandates nationwide criminal history searches rather than limiting checks to states where applicants previously resided. This federal legislation closed critical loopholes in the previous system.
The Act requires fingerprint-based searches of FBI databases covering all 50 states. Enhanced nurse aide registry checks must now cross state lines to identify previous violations. Provider enrollment screening flags excluded individuals attempting to gain employment through relocation.
For home healthcare agencies, this means expanded screening scope. A California-based agency hiring a worker who previously lived in Florida must now conduct comprehensive checks in both states. The Act prevents workers with disqualifying convictions from simply moving to new jurisdictions to avoid detection.
FCRA Compliance for Background Screening
The Fair Credit Reporting Act (FCRA) establishes critical procedural requirements when conducting background checks through third-party consumer reporting agencies. Violations of FCRA protocols can result in penalties regardless of the background check findings. Agencies must implement specific procedures to maintain compliance.
FCRA requirements include providing written disclosure on a standalone document that a background check will be conducted. Agencies must obtain written authorization from the applicant before initiating any screening. When denying employment based on background check findings, employers must follow adverse action protocols including pre-adverse action notices. Confidentiality of background check reports must be maintained with restricted access to authorized personnel only.
FCRA violations carry penalties of $100-$1,000 per violation. Actual damages become available in cases involving willful non-compliance. Many agencies partner with FCRA-compliant background screening providers to mitigate these procedural risks and ensure proper documentation.
Disqualifying Offenses for Home Health Workers
Understanding which criminal convictions permanently or temporarily bar employment is essential for efficient applicant screening. Federal and state regulations establish different categories of disqualifying offenses based on severity and risk to vulnerable populations. Approximately 18% of home health aide applicants have at least one criminal record, making thorough screening essential.
Permanent Disqualifying Convictions
Federal and most state regulations establish lifetime bars for serious offenses that demonstrate unfitness to work with vulnerable populations. These permanent disqualifications have no lookback limitation—a conviction from 30 years ago carries the same disqualifying weight as a recent conviction.
| Offense Category | Specific Examples | Lookback Period |
| Homicide | Murder, manslaughter, vehicular homicide resulting in death | Lifetime |
| Sexual Offenses | Sexual assault, rape, sexual abuse, child molestation | Lifetime |
| Child Harm | Child abuse causing serious injury or death, child endangerment | Lifetime |
| Violent Crimes | Kidnapping, false imprisonment, arson with intent to harm | Lifetime |
| Financial Exploitation | Elder financial exploitation, guardianship abuse | Lifetime |
These offenses demonstrate such serious risk that no rehabilitation period allows reconsideration. State licensing boards maintain no waiver or exemption processes for these convictions. Employment of individuals with these convictions results in automatic agency sanctions.
Time-Limited Disqualifying Offenses
Many convictions create temporary employment bars based on lookback periods that vary by state. These periods typically range from 5-10 years from conviction or release from incarceration, whichever occurs later. Understanding these timeframes helps agencies manage conditional offers appropriately.
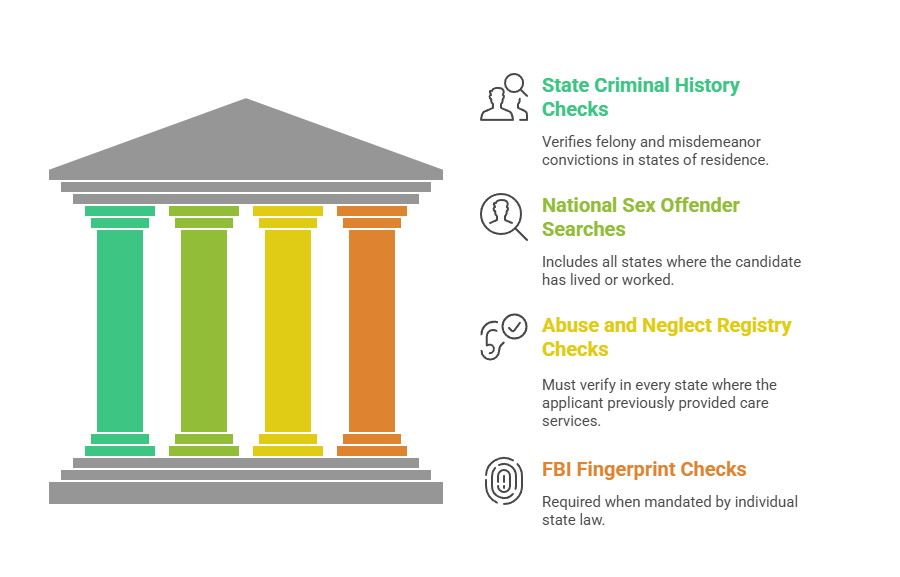
Common time-limited disqualifications include:
- Felony assault and battery: Most states apply 7-10 year lookback periods from conviction date.
- Theft, fraud, and embezzlement: Typically 5-7 year lookback periods, though some states extend to 10 years for elder financial crimes.
- Drug trafficking and distribution: Usually 7-10 year lookback periods, with lifetime bars in some jurisdictions.
- Domestic violence convictions: Range from 5-10 year lookback periods depending on severity and state law.
- Elder abuse or neglect without serious harm: Generally 7-10 year lookback periods with possible exemption processes.
Some states provide individualized assessment processes allowing applicants to petition for waiver consideration after specified waiting periods. California permits certain applicants to request exemptions after demonstrating rehabilitation evidence including completion of treatment programs and stable employment history.
State-by-State Background Check Variations
While federal requirements establish the baseline, state regulations create significant compliance complexity through additional screening mandates. The regulatory landscape varies dramatically across jurisdictions, requiring agencies to maintain state-specific protocols. Multi-state operators face the most complex compliance obligations as they navigate different requirements simultaneously.
States with the Most Stringent Requirements
Several states impose enhanced screening requirements beyond federal minimums. These jurisdictions have implemented additional layers of protection for vulnerable populations receiving home health services. Understanding these enhanced requirements prevents costly compliance failures.
- California requires comprehensive criminal background clearance through the Department of Justice and FBI fingerprinting. The state mandates Child Abuse Central Index checks and tuberculosis screening for all healthcare workers. California's lookback period is lifetime for most serious offenses, with limited exemption processes available only after extensive documentation.
- New York mandates State Criminal History Repository checks and FBI fingerprinting for certain positions. The Statewide Central Register of Child Abuse and Maltreatment must be searched for all applicants. Justice Center Background Checks apply for agencies serving developmentally disabled populations. New York requires recertification every 2 years for continuing employment.
- Texas requires Employee Misconduct Registry checks specific to Texas health and human services. Standard criminal background and abuse registry searches apply in addition to this specialized registry. Texas imposes strict 48-hour reporting requirements when agencies discover disqualifying information post-hire. Failure to report triggers automatic licensing sanctions.
- Florida implements Level 2 background screening, the most comprehensive tier available. This includes FBI fingerprinting and abuse registry checks in all states of previous residence. Florida requires re-screening every 5 years for all continuing employees. The state maintains one of the most extensive lists of disqualifying offenses in the nation.
Background Check Processing Times
Processing speed varies significantly based on state infrastructure and screening components required. Understanding typical turnaround times helps agencies plan onboarding schedules and manage candidate expectations. Delays can impact your ability to maintain adequate staffing levels during peak demand periods.
| Processing Speed | Timeline | States |
| Fastest | 3-5 business days | Georgia, Virginia, Colorado (electronic fingerprint systems) |
| Average | 7-10 business days | Most states with standard fingerprint processing |
| Slowest | 14-21+ business days | California, New York (manual verification and FBI backlogs) |
Agencies can expedite processing by using electronic fingerprint capture services. Submitting complete applications without errors requiring resubmission significantly reduces delays. Some states offer expedited processing for additional fees, reducing turnaround to 3-5 business days total.
Essential Background Screening Components

Comprehensive home health worker screening extends beyond basic criminal history to create layered protection. Modern screening programs incorporate multiple verification sources to build complete risk profiles. This multi-faceted approach provides the strongest defense against negligent hiring liability.
Core Screening Elements
A complete home care worker screening program should include criminal background checks at multiple levels. County-level searches cover all counties of residence for the past 7-10 years to capture local court records. Statewide repository searches access centralized state databases. Federal district court searches identify federal offenses not appearing in state records.
Professional verifications form the second critical screening layer:

- Certification and license verification: Direct confirmation through state nursing boards prevents credential fraud.
- Employment history verification: Coverage of past 3-5 years identifies patterns and gaps requiring explanation.
- Education verification: Confirms claimed credentials through direct source contact with institutions.
- Reference checks: Previous healthcare employers provide insight into job performance and patient interaction quality.
Specialized healthcare screenings complete the comprehensive approach. OIG LEIE monthly monitoring prevents employment of excluded individuals. State Medicaid exclusion lists must be checked separately as they don't always sync with federal databases. DEA controlled substance registration verification applies for positions involving medication administration.
Fingerprint-Based vs. Name-Based Searches
Understanding the differences between search methodologies helps agencies select appropriate screening depth. Each approach offers distinct advantages and limitations that impact accuracy and cost. The choice significantly affects your ability to identify disqualifying records reliably.
- Fingerprint-based searches provide the highest accuracy by positively identifying criminal records belonging to the specific individual. These searches eliminate false positives from name matches with different individuals. They access sealed or expunged records when state law permits employment screening use. Fingerprint searches typically cost $50-$85 and take 5-10 business days to process.
- Name-based searches rely on matching personal identifiers including name, date of birth, and Social Security number. These searches are prone to false positives when records belong to someone else with the same name. False negatives occur when records are missed due to name variations or aliases used by the applicant. While faster and less expensive at $25-$45, name-based searches alone don't satisfy federal requirements in most states.
Best practice combines fingerprint-based searches as the primary criminal background check method with multi-state database searches to identify potential records requiring further investigation. This layered approach balances accuracy with comprehensive geographic coverage.
Conditional Hiring and Pre-Clearance Protocols
Balancing rapid onboarding needs with regulatory compliance requires structured conditional hiring protocols. Labor shortages in home healthcare create pressure to expedite hiring timelines. However, premature patient contact creates serious liability and regulatory risks that agencies must carefully manage.
Permissible Pre-Clearance Activities
Federal regulations explicitly prohibit direct patient care activities before background check clearance. CMS defines "direct patient access" as physical interaction, access to patient records, or entry into patient homes. All these activities remain prohibited for conditional employees awaiting clearance.
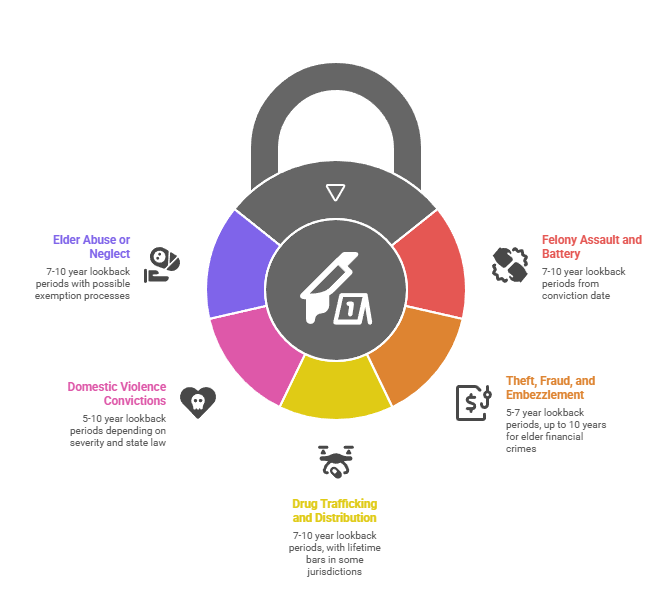
While awaiting background check results, agencies may conditionally employ workers for specific activities:
- Orientation and compliance training: Covers HIPAA, safety protocols, infection control, and agency policies without patient involvement.
- Skills competency assessments: Hands-on training with mannequins and simulation equipment in controlled environments.
- Administrative onboarding: Payroll setup, uniform ordering, scheduling system training, and completion of employment paperwork.
- Supervised observation: Watching patient care provided by cleared employees without independent patient contact or record access.
These activities allow productive use of the waiting period while maintaining strict compliance. Agencies should document all conditional employment activities to demonstrate compliance during audits. Clear policies preventing patient contact must be communicated to conditional employees and supervising staff.
Supervision Requirements During Conditional Employment
When state law permits limited patient exposure during the clearance waiting period, strict supervision protocols must be implemented. Only 12 states permit any level of supervised patient contact before full clearance. Agencies should consult state-specific regulations before implementing supervised conditional employment models to avoid violations.
Permitted supervision models require line-of-sight supervision where a fully cleared employee maintains visual contact at all times. Conditional employees cannot be scheduled for solo visits or left alone with patients under any circumstances. Daily supervision logs must document activities performed and supervisor observations throughout each shift. Restricted duties limit conditional employees to basic assistance tasks under direct instruction from cleared supervisors.
Compliance Documentation and Audit Preparedness
Proper documentation creates defensible audit trails and protects agencies from negligent hiring claims. State licensing surveys and Medicare certification audits regularly examine background check compliance. Deficiencies discovered during audits can result in conditional licensure status, civil monetary penalties, or certification termination in severe cases.
Required Retention and Documentation
Home health agencies must maintain comprehensive screening documentation for each employee. Background check files must contain original FCRA disclosure and authorization forms with applicant signatures. Complete background check reports from all sources must be retained including criminal history, abuse registries, and exclusion list results.
Documentation requirements include:
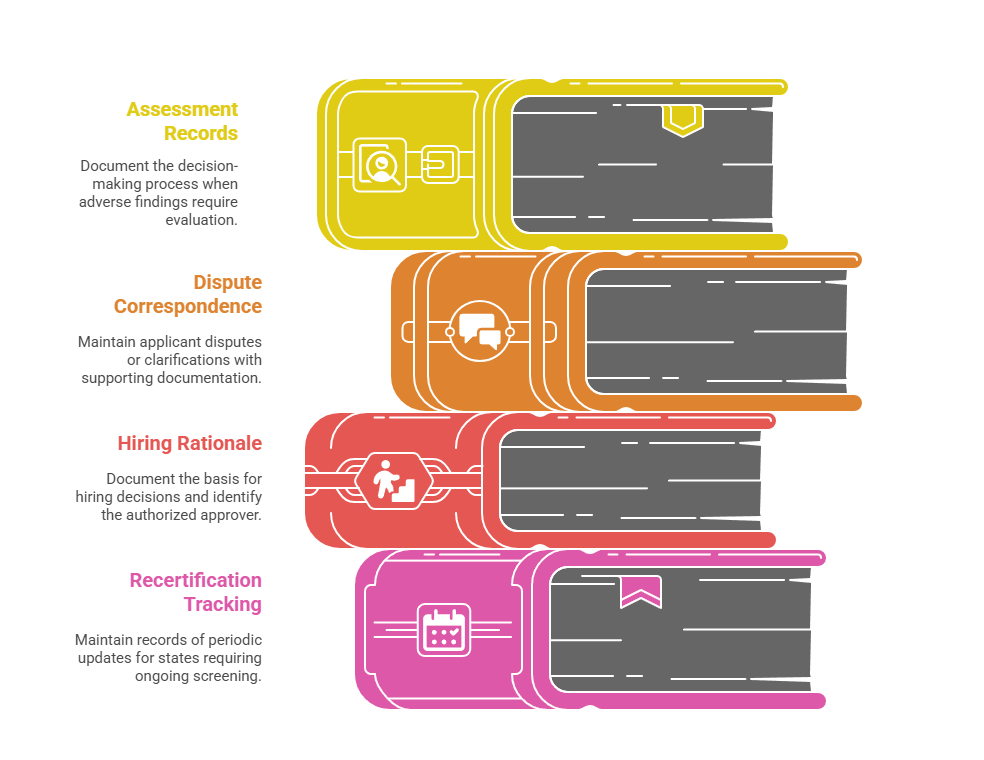
- Individualized assessment records: When adverse findings require evaluation, document the decision-making process and factors considered.
- Dispute correspondence: Any applicant disputes or clarifications must be maintained with supporting documentation.
- Final hiring decision rationale: Document the basis for hiring decisions and identify the authorized approver.
- Recertification tracking: For states requiring ongoing screening, maintain clear records of all periodic updates.
Federal regulations require 3-year retention of employee screening files. Many states mandate 5-7 years retention periods. Best practice is 7-year retention to align with most statute of limitations periods for negligent hiring claims. FCRA requires background check documentation to be stored separately from general personnel files with restricted access.
Negligent Hiring Liability Protection
Comprehensive background screening provides critical protection in negligent hiring litigation. Negligent hiring claims arise when an employee harms a patient and the plaintiff alleges the agency failed to conduct reasonable pre-employment screening. Damages in successful negligent hiring cases average $1.2 million according to recent industry data.
To successfully defend negligent hiring claims, agencies must demonstrate reasonable screening procedures appropriate to the position's responsibilities. Consistent application of screening policies across all hires proves non-discriminatory practices. Individualized assessment of identified risks shows thoughtful decision-making rather than blanket exclusions. Proper documentation of screening and decision-making processes provides the evidentiary foundation for defense.
Partnering with accredited background screening providers who maintain Professional Background Screening Association (PBSA) accreditation adds an additional layer of compliance protection. These providers follow industry best practices and maintain comprehensive quality assurance programs. Their expertise in FCRA compliance and adverse action procedures reduces your procedural risk significantly.
Cost Analysis and Vendor Selection
Understanding background check investment helps agencies budget appropriately and select cost-effective screening partners. Comprehensive screening represents a significant operational expense that must be balanced against regulatory requirements and liability protection. Strategic vendor selection can reduce costs while maintaining thorough compliance.
Typical Cost Breakdown
Comprehensive home health aide background screening includes multiple components that each carry separate costs. Understanding this breakdown helps agencies evaluate vendor proposals and identify potential hidden fees. Total investment varies based on state requirements and the depth of screening selected.
| Screening Component | Cost Range | Frequency |
| Basic criminal background check | $25-$45 | Per hire |
| FBI fingerprint processing | $45-$75 | Per hire (varies by state) |
| Abuse registry searches | $10-$25 per state | Per hire |
| License verification | $15-$30 per credential | Per hire |
| Ongoing monitoring services | $24-$60 | Annual per employee |
| Drug screening | $35-$75 | When required |
Total per-hire investment ranges from $150-$300 for comprehensive initial screening. Annual recertification costs add $75-$150 per employee in states requiring ongoing monitoring. For a 50-employee agency with 30% annual turnover, expect annual screening costs of $6,750-$13,500 including initial screenings for 15 new hires plus recertification for continuing employees.
Background Check Provider Evaluation
When selecting screening vendors, agencies should evaluate compliance credentials, service capabilities, support quality, and technology platforms. PBSA accreditation demonstrates adherence to industry best practices and quality standards. FCRA compliance guarantees and adverse action support protect agencies from procedural violations.
Service capabilities should include turnaround time guarantees with service level agreements specifying maximum processing days. Electronic fingerprint submission options significantly reduce processing time compared to paper cards. Automated abuse registry searches across all states eliminate manual verification delays. Integrated applicant tracking system compatibility streamlines workflow and reduces data entry.
Support and transparency differentiate quality providers from budget options. Dedicated healthcare industry account management provides expertise in regulatory requirements. Transparent pricing without hidden fees allows accurate budget forecasting. Comprehensive candidate dispute resolution support protects agencies during FCRA adverse action processes. Audit support and documentation assistance proves valuable during licensing surveys.
Conclusion
Home health aide background check requirements represent a complex intersection of federal mandates and state-specific regulations that demand careful navigation. Comprehensive screening programs that exceed minimum compliance standards satisfy regulatory obligations while providing essential liability protection. As regulatory scrutiny intensifies and states continue implementing enhanced requirements, partnering with experienced providers becomes increasingly critical. Investing in robust screening infrastructure protects your agency from costly compliance failures and positions your organization as a trusted care provider.
Frequently Asked Questions
How long does a home health aide background check take?
Most home health aide background checks take 7-14 business days to complete, depending on screening components required in your state. FBI fingerprint processing typically takes 3-5 business days, while state criminal repository checks process within 3-7 days. Abuse registry verifications add 2-5 days, particularly when searching multiple states. Electronic fingerprint submission significantly reduces processing time compared to paper card submissions.
Can home health aides work while waiting for background check results?
Federal regulations prohibit home health aides from providing direct patient care or accessing patient information before background check clearance. Agencies may employ candidates conditionally for orientation, training, and administrative activities without patient contact. Some states permit supervised patient contact with line-of-sight supervision by a fully cleared employee. Verify your specific state regulations regarding permissible conditional employment activities.
What disqualifies someone from being a home health aide?
Permanent disqualifying offenses include murder, sexual assault, child abuse causing serious harm, kidnapping, and arson. Time-limited disqualifications apply to felony assault (7-10 year lookback), theft and fraud (5-7 years), drug trafficking (7-10 years), and domestic violence (5-10 years). Candidates listed on the OIG exclusion list, state Medicaid fraud registries, or abuse registries are also disqualified. Each state maintains detailed lists of disqualifying offenses in their licensing regulations.
Do home health agencies check employment history?
Yes, comprehensive screening should include employment history verification covering the past 3-5 years, emphasizing previous healthcare positions. While not always explicitly required by regulation, employment verification serves as an essential component of reasonable hiring practices. Agencies should verify dates of employment, position titles, eligibility for rehire, and reason for separation. Previous healthcare employers provide valuable information about job performance and patient interaction quality.
Are FBI fingerprint checks required for home health aides in all states?
FBI fingerprint requirements vary by state, though the trend moves toward universal fingerprint-based background checks. Currently, 38 states explicitly require FBI fingerprint checks for home health aides. The 21st Century Cures Act encourages nationwide adoption of fingerprint-based screening for all long-term care workers. Even in states where not legally mandated, fingerprint-based searches represent best practice by providing the most accurate criminal history information.
How much do background checks cost for home health workers?
Comprehensive home health aide background checks typically cost $150-$300 per candidate for initial screening. This includes FBI fingerprints ($45-$75), state criminal history searches ($25-$45), abuse registry checks ($10-$25 per state), and license verifications ($15-$30). Ongoing monitoring services add $24-$60 annually per employee. Agencies conducting high volumes may negotiate volume discounts with screening providers.
What happens if a disqualifying offense is discovered after hiring?
If a disqualifying offense is discovered after hire, agencies must immediately remove the employee from patient care duties and initiate termination procedures. Most states require reporting discovered disqualifying offenses to licensing authorities within 24-72 hours. The employee should be given the opportunity to dispute the accuracy consistent with FCRA requirements. Continued employment creates significant liability exposure and regulatory violations.
Do background check requirements differ for independent home health aides?
Independent contractors and agency-employed home health aides face the same background check requirements when providing services to Medicare/Medicaid beneficiaries or when state licensing laws apply. Enforcement mechanisms differ—agencies face license revocation and Medicare decertification for non-compliance, while independent contractors may face individual sanctions. Families privately hiring independent aides should still conduct comprehensive background screening to protect vulnerable family members.
Additional Resources
- CMS Background Check Requirements for Long-Term Care Facilities
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-13-32.pdf - National Background Check Program State-by-State Guide
https://www.ncsl.org/research/human-services/background-checks-for-childcare.aspx - FTC Fair Credit Reporting Act Compliance Guide for Employers
https://www.ftc.gov/tips-advice/business-center/guidance/using-consumer-reports-what-employers-need-know - OIG List of Excluded Individuals and Entities Database
https://oig.hhs.gov/exclusions/index.asp - Professional Background Screening Association Best Practices
https://www.psbassociation.org/standards-best-practices

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.