Navigating the complex landscape of consent and disclosure in healthcare screening can be challenging. Healthcare professionals and employers must adhere to a complex set of laws and regulations designed to protect the rights of employees while ensuring a safe and trustworthy work environment. This comprehensive guide will cover everything you need to know about background check consent in healthcare, FCRA compliance, and the intricacies of HIPAA and adverse actions.
Key Takeaways
- Consent and disclosure are essential for legal and ethical healthcare background checks.
- FCRA compliance is crucial in ensuring that your background check procedures meet federal regulations.
- Proper handling of adverse action notices is important to maintain fairness and avoid legal issues.
- Pre-employment screening in healthcare requires strict adherence to both federal and state regulations.
- HIPAA compliance during background checks is necessary to protect patient information and maintain trust.
Introduction
Consent and disclosure are pivotal in healthcare background checks. They ensure that employee rights are protected while maintaining a safe workplace. Key concepts like "background check consent healthcare" and "FCRA compliance healthcare" clarify this process. The goal here is to provide a clear roadmap for navigating these regulations, empowering you with the understanding needed to align your practices with legal standards. Whether you're an employer, healthcare professional, or both, knowing these rules is essential to fostering trust and compliance. If we understand why we have the laws and not the laws alone, we recruit more openly and honestly. This handbook is designed to enable you to comply with the laws on a day-by-day basis and keep in mind the important people.
Understanding Background Check Consent in Healthcare
Consent is the foundation of any background check process, particularly in healthcare. When you, as an employer or healthcare organization, initiate a background check, obtaining explicit consent from the individual involved is not just good practiceâitâs a legal requirement. This means informing the individual clearly and obtaining their permission before proceeding with any background screening.
Legal requirements for obtaining consent are defined by specific legislation. The Fair Credit Reporting Act (FCRA) is central in guiding how background check consent must be obtained and handled. Under the FCRA, you must provide a clear and conspicuous disclosure, separate from other documents and in a written format, saying that a background check will occur. The individual must provide written authorization for the check to proceed. It's critical that this consent isn't hidden within other application materials or employment forms.
A background check consent form plays a pivotal role in this process. This form needs to be straightforward and should include details such as the scope of the background check and the entities involved in conducting it. You should ensure that the form is easy to understand and avoids legal jargon that could confuse the applicant. The consent form also acts as documentation, providing a record that consent was properly secured, which is crucial for legal protection.
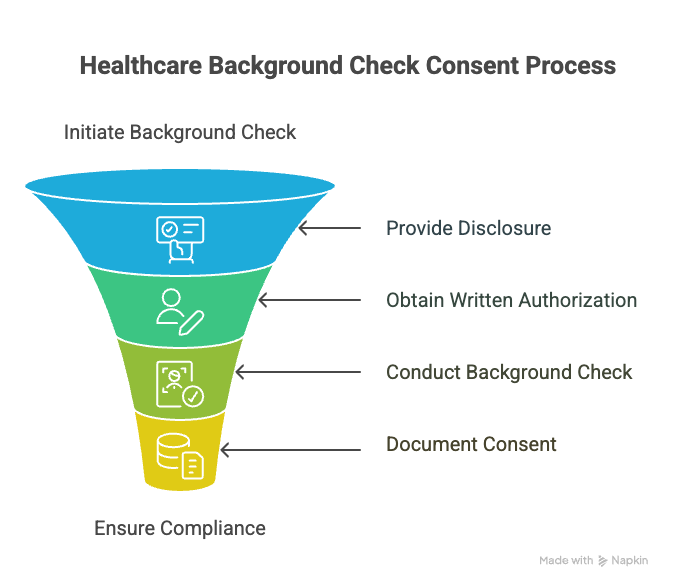
When constructing a consent process, ask yourself if the communication is as clear as it could be. Does the individual know exactly what they're consenting to, and are they doing so willingly? Make sure that your process respects individual rights while aligning with regulatory frameworks. Meeting these standards helps build trust and ensures compliance, reducing the risk of future legal complications.
FCRA Compliance in Healthcare
The Fair Credit Reporting Act (FCRA) is a federal law that governs the collection and use of consumer information, and it plays a critical role in healthcare background checks. If you're a healthcare employer, understanding FCRA compliance is crucial because it ensures that the background checks you perform are legal and ethical.
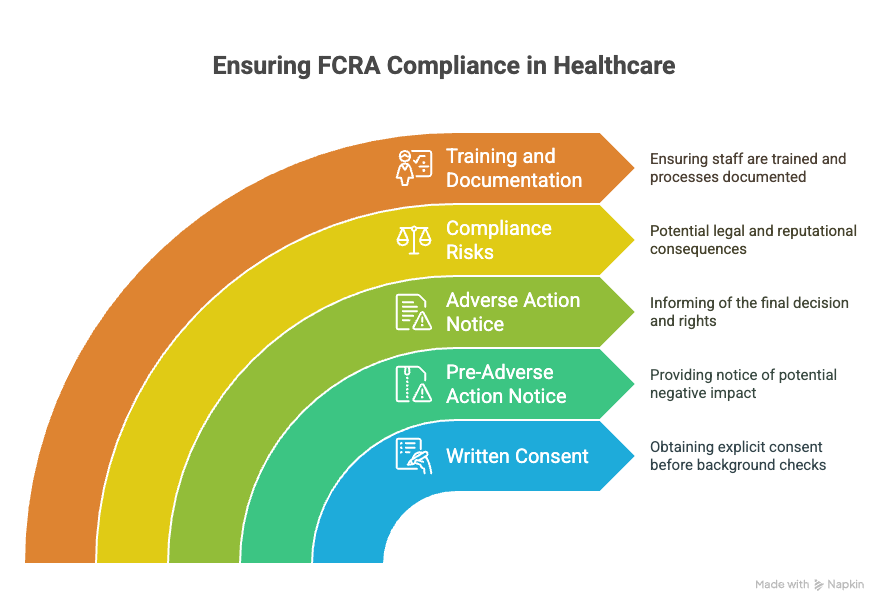
Healthcare organizations must obtain written consent from individuals before conducting a background check. This is a non-negotiable prerequisite of the FCRA. You should provide a clear and separate disclosure explaining that you will obtain a consumer report for employment purposes. Mixing this consent with other application materials can lead to compliance issues.
Another FCRA requirement is the provision of a "pre-adverse action" notice if the background check reveals information that might negatively impact a hiring decision. This notice should include a copy of the report and a summary of the individual's rights under the FCRA. This step gives the applicant a chance to review the report and correct any inaccuracies.
A common mistake is skipping the "adverse action" notice, which is sent if you decide not to hire someone based on the report findings. This final notice confirms the decision and informs the applicant of their rights, such as the right to contest the report's accuracy.
FCRA violations can lead to lawsuits and damage your organization's reputation. Have you ensured that your processes align with FCRA requirements? Double-check your consent forms, and make sure your team is trained on proper notification procedures. It's an investment in compliance that protects both your organization and the individuals you hire.
Adverse Action in Healthcare Screening
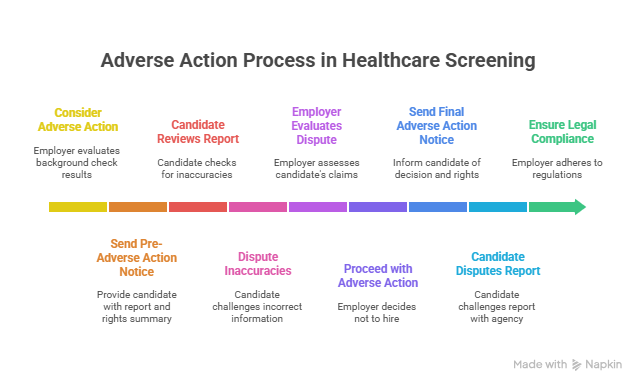
Adverse action occurs when an employer decides against hiring a candidate based on information found during a background check. This can include both criminal records and credit history. In healthcare, adverse actions must be handled with particular care due to the sensitive nature of the work.
The procedure for adverse action involves a few key steps. First, if you're considering taking adverse action, you must provide the individual with a pre-adverse action notice. This includes a copy of the background check report and a summary of their rights under the Fair Credit Reporting Act (FCRA). This gives the candidate a chance to review the report and dispute any inaccuracies before a final decision is made.
After a reasonable period, if no changes are warranted, you may proceed with the adverse action. You must send a final adverse action notice, informing the applicant of the decision not to hire them. This notice must include information on the company that provided the background check report, a statement that the company did not make the adverse decision, and the candidateâs right to dispute the reportâs accuracy with the reporting agency.
Legal considerations are critical. Failure to follow the correct procedure can lead to legal trouble, including lawsuits and fines. Always ensure compliance with both federal and state regulations to protect your organization. Have you reviewed your adverse action procedures lately? Keeping them updated not only protects you legally but also fosters a fair hiring process.
Pre-Employment Screening Regulations
Pre-employment screening lays the foundation for a secure healthcare environment. In healthcare, where patient safety and trust are paramount, ensuring that employees have clean records and the necessary qualifications is critical.
Regulations governing pre-employment screening in healthcare are stringent and multifaceted. At the federal level, the Equal Employment Opportunity Commission (EEOC) and the Fair Credit Reporting Act (FCRA) set out broad rules applicable across industries. However, healthcare has additional layers, like the Office of Inspector Generalâs (OIG) exclusion list, which employers must consult to ensure potential hires are not sanctioned.
Key pre-employment regulations include verifying credentials and licenses, checking criminal records with an understanding of both time-sensitive and comprehensive background histories, and screening for drug use, as stipulated by the Drug-Free Workplace Act for those holding federal contracts.
Adopting best practices can streamline compliance. First, always use standardized consent forms to inform candidates clearly about the checks to be conducted. This transparency builds trust and ensures legal compliance.
Next, be diligent about exploring both federal and state-specific requirements. Each state may have its unique laws, and staying informed about these can prevent costly missteps.
Another practice involves using reputable background check providers who understand the nuances of healthcare screening. They can assist in executing searches that are thorough yet respect privacy and consent rules.
Finally, establish a system for regular training sessions to keep your HR team sharp on the latest regulations and ethical standards. Healthcare regulations evolve, and keeping your policies adaptable is essential for compliance and operational integrity.
Healthcare Screening Laws
Federal laws set the baseline for healthcare screening. The Fair Credit Reporting Act (FCRA) and Equal Employment Opportunity Commission (EEOC) guidelines play significant roles. These require that you gather candidate consent and provide disclosures if adverse actions result from screenings. Healthcare settings often involve safety-sensitive roles, which means extra scrutiny is needed. You can reference the Department of Laborâs resources for comprehensive guidance on these federal requirements.
State laws can complicate things. While federal regulations provide a framework, states often impose their own rules. For instance, Californiaâs Investigative Consumer Reporting Agencies Act (ICRAA) places stricter limits on the types of information employers can access and how they notify job candidates. Staying updated on your specific stateâs legislation is crucial, as failing to comply can lead to legal issues and penalties.
Recent legal developments include increased data protection measures and evolving definitions of permissible checks. As technology advances, states are tightening rules around how data is accessed and stored, particularly for sensitive roles involving patient care. Make sure you regularly review changes in both federal and state laws to maintain compliance.
Understanding these layers of regulation requires attention to detail and proactive management. Keeping up with legal shifts not only protects your organization but also fosters an environment of trust and safety for all staff and patients.
HIPAA and Background Checks
HIPAA, or the Health Insurance Portability and Accountability Act, sets national standards for protecting sensitive patient information. In healthcare, maintaining privacy is paramount. But where does this leave background checks, which are crucial for hiring trustworthy healthcare professionals?
HIPAA primarily aims to protect patient information from unauthorized access. This extends to background checks. When conducting these checks, healthcare employers must ensure they're not compromising patient data. This means understanding how HIPAA rules apply to the hiring process.
Background checks in healthcare often necessitate accessing various records. This can include professional credentials or history that might intersect with patient information. Healthcare employers must ensure any used data remains separate from HIPAA-protected information. A breach in this area could lead to severe legal consequences.
Here's how you can maintain compliance: keep patient data and employee data separate at all stages of the hiring process. Use only information relevant to the job role while ensuring all data handling aligns with HIPAA standards. Educate staff about the importance of this separation and invest in secure data management systems.
It's essential to have detailed protocols in place. Regular training and audits can help keep your processes aligned with HIPAA. Avoid gray areas by consulting with legal experts when in doubt. A rule of thumbâif any part of the process feels like it might risk patient privacy, it probably does.
Do your background check protocols respect HIPAA requirements? If not, it's time to review your procedures. Understanding and applying these standards is not just about legal compliance; it's about fostering trust and integrity in your healthcare organization.
Resources
When it comes to getting a deeper understanding of background checks in healthcare, keeping reputable resources at your fingertips is crucial. Direct access to trusted materials simplifies your path to compliance and enhances your knowledge base. Here are some resources that will be beneficial:
- Common Background Check Questions: For answers to frequently asked questions about background checks, you can refer to the article "Most Common Background Check Questions". It provides straightforward explanations and could help clarify any doubts you may have.
- Fair Credit Reporting Act (FCRA) Insights: Dive into authoritative sources, like the Federal Trade Commission's (FTC) website, to review the text of the FCRA and understand its application in healthcare. Accurate information leads to better implementation.
- HIPAA Guidance: Review the "U.S. Department of Health & Human Services" for clear guidelines on maintaining patient privacy and meeting HIPAA requirements while conducting background checks.
- State-Specific Regulations: Since state laws can vary significantly, itâs useful to consult your state's labor department website. This ensures you remain compliant with local laws besides federal regulations.
- Pre-Employment Screening Tips: Consider checking out the Society for Human Resource Management (SHRM) for best practices in pre-employment screenings within healthcare settings.
These resources will aid you in aligning your screening processes with current legal standards. Always stay informed to avoid compliance pitfalls and ensure the integrity of your hiring practices.
Conclusion
You now have a clearer understanding of the intricacies involved in healthcare screening. Keeping up with consent, FCRA compliance, and adverse action procedures is not just about following rules. It's about ensuring a fair and safe workplace. Review your current practices. Are they up to date with the latest laws? Small adjustments can make a big difference. Prioritize compliance today. Stay informed, stay compliant, and protect your organization and its people. Your diligence now can prevent headaches later on. Embrace these practices for a more trusted healthcare environment.
Frequently Asked Questions (FAQs)
Is consent required for healthcare background checks?
Yes, consent is necessary. You must obtain written permission from the candidate before conducting a background check.
What should be included in a background check disclosure form?
The form must clearly state that a background check will be conducted. It should include details like the type of checks, the scope of the inquiry, and the candidateâs rights.
What is the FCRA requirement for healthcare employers?
The Fair Credit Reporting Act (FCRA) requires employers to provide a clear and conspicuous disclosure, obtain written consent, and give applicants a copy of the report if an adverse decision is made based on the results.
Do hospitals need written permission for background checks?
Yes, hospitals must obtain written consent from the applicant to perform background checks, in compliance with FCRA guidelines.
Can you run a background check without informing the candidate?
No, you cannot. Candidates must be informed and provide written consent. Failing to do so may lead to legal issues.
Are there specific checks required for healthcare professionals?
Yes, checks often include verification of licenses, criminal records, and employment history due to the sensitive nature of the field.
How long does a healthcare background check usually take?
Typically, it takes between 3 to 5 business days. However, complex checks may take longer.
Can a candidate dispute the result of a background check?
Yes, candidates have the right to dispute inaccuracies in their background check report. They should contact the reporting agency to begin the dispute process.
What should you do if an error is found in your background check?
Contact the background check provider immediately to address the error. Provide documentation that supports your claim for correction.
Definitions
Background Check Consent
This is written permission from a job candidate allowing an employer to conduct a background check. You must provide a clear, standalone disclosure before getting this consent. The form should explain what the screening includes, who performs it, and how the results are used. Never bury consent inside larger packets or application materials. Doing so risks legal issues and breaks trust with the applicant.
FCRA Compliance
FCRA stands for Fair Credit Reporting Act. It sets federal rules for how background checks are handled. Following FCRA means giving clear notice, getting written consent, and sending required notificationsâespecially if you make a negative hiring decision based on the report. Ignoring FCRA rules can lead to legal penalties and harm your reputation. Are your hiring and screening steps following these legal basics?
Adverse Action
This is the process of rejecting a job candidate based on the results of their background check. It involves two steps: first, a "pre-adverse action" notice with a copy of the report and a summary of rights. After giving the candidate time to respond, you may send a final "adverse action" notice. Skipping these steps violates federal law. Has your team reviewed how these notices are issued?
Pre-Employment Screening
This refers to checks done before hiring someone. In healthcare, it often includes verifying licenses, checking for criminal records, reviewing drug test results, and consulting exclusion lists like the OIGâs. The goal is to ensure candidates meet safety, legal, and ethical standards. Do your screening steps align with both federal and local laws?
HIPAA
HIPAA stands for the Health Insurance Portability and Accountability Act. It protects sensitive patient information. When running background checks, you can't use or expose data that falls under HIPAA unless absolutely necessary. Keep applicant data separated from patient data. Are your hiring records stored in a way that respects this boundary?
Reference
- University of Washington CHWS Report:
https://familymedicine.uw.edu/chws/wp-content/uploads/sites/5/2021/11/Background-Checks-FR-2021.pdf

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.