In the healthcare industry, ensuring the privacy and security of background check data is crucial. With rising concerns over data breaches and privacy violations, understanding and complying with regulations such as HIPAA (Health Insurance Portability and Accountability Act) is more important than ever. This guide explores how HIPAA and other regulations affect background check data privacy in healthcare settings, offering insights for both employers and employees.
Key Takeaways
- HIPAA requires strict safeguards to protect personal health information during healthcare background checks.
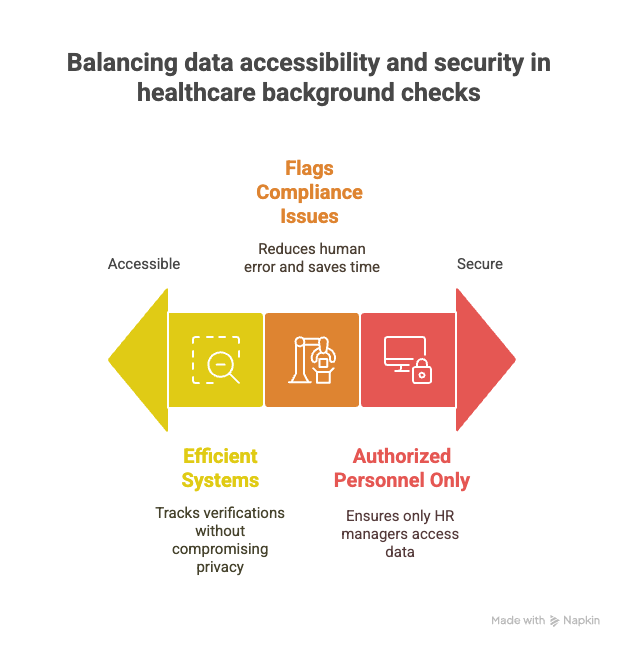
- Balancing data accessibility and privacy is crucial for HR teams conducting background checks in healthcare.
- Compliance with multiple privacy laws, like GDPR and CCPA, is necessary for handling data effectively.
- Employing encryption and strong access controls helps ensure the security of sensitive healthcare data.
- Regular audits, ongoing staff training, and clear data privacy policies play vital roles in protecting background check data.
Introduction
Data privacy in healthcare is becoming increasingly important. The sector handles sensitive information, and keeping it secure is non-negotiable. Healthcare information is not just medical records. It involves background checks for new employees, too. So, how do you maintain privacy in this area?
This guide aims to provide a complete understanding of background check data privacy in healthcare, with a spotlight on HIPAA compliance. We'll cover key regulations, practical data protection strategies, and why HR compliance is crucial in healthcare. If you're managing healthcare data, this information is essential for you. Embrace these insights to protect data effectively and adhere to necessary regulations.
Understanding HIPAA and Its Implications
HIPAA, or the Health Insurance Portability and Accountability Act, was enacted in 1996 to protect the privacy and security of health information. It seeks to ensure that personal health data, known as Protected Health Information (PHI), is handled with utmost confidentiality and security. This federal law impacts how healthcare entities manage, store, and share information, including data collected during background checks.

HIPAA has several provisions critical to background checks. It mandates that any data collected, processed, or stored falls under strict privacy guidelines if it can be linked to a specific individual and pertains to health. For instance, if an applicant's medical records or health status is included in a background check, that data is PHI and must be safeguarded under HIPAA rules.
Real-world breaches highlight the consequences of mishandling such information. Consider the case of a healthcare provider fined heavily because an employee's background check data, which included sensitive health information, got compromised due to inadequate security measures. This incident underscores the necessity for compliance and the need for stringent controls on who accesses such data and how it is secured.
Implementing proper access controls and encrypting data are just the start; your organization must have a clear strategy for maintaining and auditing compliance. Are you confident your policies align with these requirements? Engaging in regular reviews and updates can help mitigate risks and protect your organization from significant penalties.
Background Check Data Privacy in Healthcare
Background checks in healthcare are unique given the sensitivity of the information involved. You’re not just handling names and addresses; you’re dealing with data that could include criminal histories, work experiences, and in some cases, Protected Health Information (PHI). This complexity brings unique risks and responsibilities.
A common challenge is ensuring that this data remains secure while still accessible to those who need it. For instance, HR teams require efficient systems to track verifications without compromising privacy. It’s a fine line to walk, especially when mistakes can lead to data breaches or costly legal penalties.
One practical approach is to implement strict access controls. These controls ensure only authorized personnel can see sensitive data. For instance, only HR managers might access full background checks, while others can see only what’s necessary for their role.
Balancing compliance and practicality is another hurdle. HIPAA sets high standards for PHI protection, but it’s crucial to address these requirements without grinding operations to a halt. Automated systems can help by flagging compliance issues before they become problems, saving you time and reducing human error.
It's about creating an environment where privacy is not only a legal requirement but a business practice. Have you considered how your systems handle this balance? The right approach keeps your data safe and your organization on solid ground.
Legal and Regulatory Frameworks
HIPAA isn't the only regulation you need to keep an eye on. Other frameworks also impact healthcare data privacy. The GDPR, or General Data Protection Regulation, for instance, sets standards for data protection in the EU but affects any organization handling EU residents' data, no matter where it's based. If your healthcare organization processes such data, GDPR compliance is non-negotiable. It's about synchronizing patient care with detailed documentation and stringent privacy measures.
States in the U.S. have their own rules, which can vary widely. California's Consumer Privacy Act (CCPA) is an example. It offers consumers the right to know what personal data is collected and how it's used. As these regulations evolve, so should your organization’s data strategies to maintain compliance.
These regulations shape how background checks are conducted. You must ensure any screening aligns with these laws, or you risk hefty penalties and damage to your reputation. Background check processes must be transparent, well-documented, and secure.
HR compliance is crucial in navigating these waters. Human Resources often take point in ensuring that the organization's practices align with legal requirements. Resources like those from the Professional Background Screening Association (PBSA) can be invaluable. They offer guidance on compliance and best practices, helping HR teams maintain robust programs that protect both the organization and its employees.
Data Security Practices for Healthcare Organizations
Encryption is a cornerstone of data security in healthcare. It transforms sensitive information into unreadable code, making it useless to anyone who intercepts it without the right key. Implementing strong encryption protocols for your background check data is not just smart; it's essential.
Equally important are robust access controls. Limiting who can access certain data reduces the risk of unauthorized exposure. Use role-based access to ensure that only authorized personnel can view or manage sensitive information. Ask yourself: Who really needs access, and why?
Training is another key pillar. Employees must understand data privacy and security protocols thoroughly. Regular workshops can keep data protection top-of-mind. Are your staff well-equipped to handle sensitive information?
These practices are not just about compliance—they're about building trust with patients and protecting their most personal information. Implement these measures well and you serve both legality and integrity.
PHI in Background Screening
Protected Health Information (PHI) is any information that can be used to identify a patient and relates to their health status, healthcare, or payment for healthcare. In the context of background checks, PHI is critical because it involves sensitive data that requires careful handling to avoid breaches and maintain trust.
When conducting background screenings in healthcare, handling PHI with the utmost care is crucial. This means only collecting the minimum necessary information and ensuring it's stored securely. For example, encrypt data both in transit and at rest. Use secure servers and restrict access to those who absolutely need it.
A case study that highlights effective management of PHI can be seen in how one large hospital revamped its data practices after a breach due to employees accessing records improperly. The hospital implemented role-based access controls, regular audits, and mandatory staff training about handling PHI. As a result, they significantly reduced unauthorized access incidents.
You can adapt these practices by implementing strict access controls and regularly updating training programs to keep employees aware of best practices. Remember, keeping PHI safe isn't just a legal requirement—it's about maintaining the trust of patients and protecting your organization from potential data breaches.
How to Implement a Robust Data Privacy Program
Creating a solid data privacy program in healthcare begins with clear policy development. You need to craft policies that define how background check data is collected, used, and shared. These should align with legal requirements and HIPAA guidelines. Clearly written procedures serve as a roadmap for your team and set the standard for data handling.
Regular audits and assessments play a critical role in maintaining a robust program. Conduct these audits frequently to identify gaps or weaknesses in your existing practices. They help ensure continuous compliance and enhance your organization's ability to address vulnerabilities promptly. Consistent audits demonstrate your commitment to data privacy.
A crisis management plan is vital for responding to data breaches. This plan should outline the steps for identifying, containing, and mitigating data breaches. Time is crucial when a breach occurs, so having a well-established plan can save your organization from significant fallout. Include protocols for notifying affected parties and regulatory bodies, ensuring transparency and accountability.
Implementing these practices requires dedication and consistency. By doing so, you position your organization to better manage data privacy, thereby earning the trust of both patients and employees.
Future Trends and Considerations
Data privacy regulations are on the move. You might wonder how changes, like those tied to the California Consumer Privacy Act or the European Union’s data rules (GDPR), could ripple through healthcare background checks. These shifts emphasize how vital it is to watch for updates that might alter your compliance landscape.
Tech is another area to watch. Tools like AI and machine learning are reshaping how background data is processed. They’re fast and efficient, but they come with questions about privacy. How do you ensure these technologies don't overstep legal or ethical boundaries? Staying informed about tech trends and their legal implications is crucial.
Preparing for change isn't just about knowing the rules. It's about agility in policy and practice. Regular training sessions, updated protocols, and collaboration with IT can keep your team ready for shifts. Are your data storage solutions adaptable? Is your staff trained for future challenges? These considerations can help you stay ahead in a rapidly evolving field.
Conclusion
Protecting the privacy of background check data in healthcare is an ongoing task that stands at the intersection of compliance and trust. We've broken down key regulations, from HIPAA to state laws, and explored practical strategies for keeping data secure. Consistent vigilance is essential—keep auditing processes sharp and invest in staff training to mitigate risks. Use industry resources to your advantage; they serve as vital lifelines in navigating the complex regulatory landscape.
Focus on proactive measures, not just reactive fixes. Reinforce data privacy policies and ensure they evolve alongside new technological trends and legal updates. Remember, protecting background check data isn't just about compliance—it's about maintaining patient trust and upholding the integrity of your organization.
Let's bolster our defenses. Partner with compliance experts, conduct regular audits, and engage with professional associations to remain informed and prepared. A robust privacy framework isn't a static achievement but a dynamic, ongoing commitment to security and trust in healthcare.
Frequently Asked Questions (FAQs)
Is background check data protected under HIPAA?
No, background check data is not typically protected under HIPAA. HIPAA applies to protected health information (PHI), which does not include data collected for employment purposes, such as background checks.
What are the data security requirements for background screening?
Background screening data should be protected using encryption, secure storage, regular audits, and strict access controls. Ensure only authorized personnel have access to sensitive information to maintain data integrity.
Do healthcare employers need a BAA with screening vendors?
Healthcare employers may need a Business Associate Agreement (BAA) if the vendor handles PHI. If the background check process does not involve PHI, a BAA may not be necessary.
How should hospitals handle background screening breaches?
Hospitals should immediately identify the breach's scope, notify affected individuals, and assess legal obligations. Implement corrective actions and strengthen security measures to prevent future breaches.
What makes a background check vendor HIPAA-compliant?
A HIPAA-compliant vendor should use strong encryption, access controls, and data protection measures. The vendor should also train staff on HIPAA rules and be prepared to sign a BAA if handling PHI.
How often should background checks be updated?
Updates to background checks depend on your industry and role-specific requirements. Many employers choose to conduct checks annually or upon role changes.
Can candidates request copies of their background check reports?
Yes, under the Fair Credit Reporting Act (FCRA), candidates can request a copy of their background check report from the screening company used by the employer.
What should you do if a background check contains errors?
If you find an error in a background check, contact the screening company to dispute the inaccuracies. Provide documentation to support your claim and follow up for a resolution.
What information is typically included in a background check?
Background checks may include criminal records, employment history, educational qualifications, and credit history. However, the specifics can vary depending on the job and employer.
Are social media profiles part of the background screening process?
Some employers review social media profiles to gain insights into a candidate's behavior and character. Ensure any social media review complies with privacy laws and respects non-discrimination standards.
Definitions
HR Compliance
HR compliance means following employment laws and workplace regulations. In healthcare, this includes data protection laws like HIPAA and background screening rules. HR teams must ensure that hiring processes, including background checks, meet both federal and state standards. Failure to comply can lead to legal and financial penalties. Is your HR team trained on these requirements?
Background Checks
Background checks are a routine part of hiring in healthcare. They verify a candidate’s history—criminal records, work experience, certifications, and sometimes health-related data. These checks help protect patients and maintain a safe workplace. Are your background processes secure and documented
Protected Health Information (PHI)
PHI is any health-related data tied to an individual. It includes records about medical treatments, diagnoses, and insurance. If this information turns up during a background check, it's subject to HIPAA. Make sure you store and share it only when needed—and only with authorized staff.
Access Controls
Access controls limit who can see or use sensitive information. In HR, this means only certain roles—like managers or compliance officers—can view full background reports. Good access controls help prevent data leaks and support legal compliance. Who in your team can access what—and why?
Employee Training
Employee training prepares staff to handle private data correctly. In healthcare HR, this means teaching staff about HIPAA, secure data management, and breach reporting. Ongoing training reduces errors and builds a culture of responsibility. Are your staff up-to-date with data privacy policies?
References
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub
DOT Physical Requirements for Drivers: 2026 Compliance Guide
9 Jan, 2026 • 17 min read
Healthcare Employee Background Check: What Employers Need to Know in 2026
9 Jan, 2026 • 19 min read
How Long Do Background Checks Take for Government Jobs? Timeline Expectations for 2026
6 Jan, 2026 • 20 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.

