HIPAA compliant employee screening is a mandatory process that healthcare organizations must implement to protect patient privacy while meeting federal regulations during hiring and background verification. Healthcare practices face unique screening challenges that extend beyond standard employment checks, requiring specialized procedures that verify credentials, assess security risks, and ensure all staff handling protected health information (PHI) meet stringent privacy and security standards.
Key Takeaways
- HIPAA compliant employee screening requires verifying credentials, conducting privacy-focused background checks, and documenting security risk assessments before granting access to protected health information.
- Healthcare practices must obtain written authorization from candidates before accessing any health information during screening, and can only request medical records when directly relevant to essential job functions.
- Criminal background checks for healthcare positions should focus on offenses relevant to patient safety and data security, including fraud, theft, violence, and drug-related convictions.
- Credential verification for clinical staff must confirm active licenses, DEA registrations, malpractice insurance, and exclusion list status through primary sources rather than candidate-provided documentation.
- Small healthcare practices can maintain HIPAA compliance during screening by implementing standardized checklists, designated privacy officers, and secure document management systems.
- The Office for Civil Rights enforces HIPAA violations during employment screening with penalties ranging from $100 to $50,000 per violation, with annual maximums exceeding $1.5 million.
- Healthcare employers must complete HIPAA security risk assessments for new hires before granting system access, evaluating their access needs using minimum necessary standards.
- Proper employee screening reduces medical identity theft risks, prevents unauthorized PHI disclosure, and protects practices from both regulatory penalties and reputational damage.
Understanding HIPAA Compliant Employee Screening Requirements
HIPAA compliant employee screening goes far beyond traditional employment background checks. Healthcare organizations must balance thorough candidate evaluation with strict privacy protections that apply even during the hiring process. The Health Insurance Portability and Accountability Act establishes specific requirements for who can access patient information and under what circumstances, making healthcare clinic staff verification procedures fundamentally different from other industries.
The stakes are exceptionally high for healthcare practices. According to the Department of Health and Human Services, insider threats account for approximately 58% of healthcare data breaches. Many incidents involve employees who should never have been granted access to sensitive systems. For small healthcare clinics operating with limited HR resources, implementing compliant screening procedures protects both patients and the practice itself from devastating financial and reputational consequences.
The Legal Framework for Healthcare Employee Screening
HIPAA's Privacy Rule and Security Rule create specific obligations during employee screening that many healthcare practices overlook. The Privacy Rule governs how covered entities can use and disclose protected health information during the hiring process. Meanwhile, the Security Rule requires organizations to implement workforce security measures including authorization and supervision procedures.
Covered entities must designate a privacy officer and security officer who oversee the screening process. These roles can be combined in smaller practices. These individuals ensure that background checks, reference verifications, and credential confirmations occur through HIPAA-compliant channels. The screening process itself becomes part of your practice's required documentation demonstrating compliance with workforce security standards during audits or investigations.
As HR professionals, I’ve learned that the importance of trust builds long before that first day of employment. Background checks involve much more than federal regulations—protecting individuals, as well as purposes, is what this process is all about. It may involve a client’s information as a patient or as a prospective employee. Each process that we choose to follow ultimately comes down to respect for the life that is associated with a piece of paperwork.
Key Differences Between Healthcare and General Employment Screening
Healthcare screening differs substantially from standard employment verification in several critical ways. Medical practice employee screening processes must verify professional licenses, specialty certifications, hospital privileges, malpractice claims history, and exclusion from federal healthcare programs. These requirements extend far beyond typical criminal history and employment verification.
The Office of Inspector General (OIG) and System for Award Management (SAM) exclusion checks represent mandatory screening steps unique to healthcare. Hiring an excluded individual—even unknowingly—can result in severe penalties. These include loss of Medicare and Medicaid reimbursement for any services involving that employee. These databases require monthly monitoring throughout employment, not just at hiring, creating ongoing verification obligations.
Essential Components of HIPAA Compliant Background Checks
Conducting background checks for healthcare positions requires specific procedures that protect candidate privacy while gathering information necessary for patient safety. The screening process must be job-relevant, proportionate to the position's access to protected health information, and conducted through secure channels. Small healthcare business hiring requirements should follow a standardized approach that treats all candidates consistently while adjusting scope based on role-specific requirements.
A front desk receptionist who schedules appointments requires different screening depth than a nurse practitioner who diagnoses conditions and accesses complete patient records. Documenting these role-based screening tiers demonstrates the "minimum necessary" standard that HIPAA requires. Patient safety screening protocols demand this tailored approach.
| Position Level | Required Screening Components | Estimated Timeline |
| Clinical Providers (MD, NP, PA) | Multi-state criminal check, DEA/license verification, NPDB query, exclusion screening, malpractice verification, credential confirmation | 14-21 business days |
| Allied Health (RN, LPN, Medical Assistants) | Criminal background check, license verification, exclusion screening, employment verification, reference checks | 7-14 business days |
| Administrative Staff with PHI Access | Criminal check (fraud/theft focus), exclusion screening, employment verification, reference checks | 5-10 business days |
| Support Staff (minimal PHI exposure) | Basic criminal check, employment verification, reference checks | 3-7 business days |
Criminal Background Check Considerations
Criminal history screening for healthcare positions focuses on offenses that indicate risk to patients, protected health information, or practice assets. Healthcare practices should establish clear policies about which convictions disqualify candidates and which require individualized assessment. This includes considering factors like time elapsed, rehabilitation evidence, and position responsibilities.
Many states have enacted "ban the box" legislation limiting when criminal history can be requested during hiring. Healthcare employers must navigate these state-specific restrictions while maintaining patient safety standards. Generally, HIPAA and patient safety regulations provide exceptions allowing healthcare organizations to conduct criminal screenings earlier in the process than other industries. However, specific timing requirements vary by jurisdiction.
Drug Screening and Medical Information
Pre-employment drug testing in healthcare settings creates unique HIPAA considerations. While employers can require drug screening as a condition of employment, test results constitute protected health information that must be handled with strict confidentiality. Only designated personnel with legitimate need should access results. Medical review officers should communicate directly with candidates about positive results potentially explained by prescription medications.
Healthcare practices cannot request candidates' complete medical records or require disclosure of all health conditions during screening. The Americans with Disabilities Act (ADA) prohibits medical inquiries and examinations until after a conditional job offer. Post-offer medical evaluations must be job-related and consistent with business necessity, focusing on the candidate's ability to perform essential functions with or without reasonable accommodation.
Credential and License Verification Procedures
Credential verification represents perhaps the most critical component of healthcare clinic staff verification procedures. False credentials in healthcare appear with alarming frequency—the Association of Certified Fraud Examiners reports that approximately 34% of job applications contain credential misrepresentations. In healthcare, where unqualified practitioners can cause patient harm, thorough verification isn't optional.
Small healthcare business hiring requirements for credential verification demand primary source confirmation rather than accepting diplomas, certificates, or candidate attestations. Primary source verification means contacting the issuing institution, licensing board, or certification organization directly. Third-party verification services can streamline this process while maintaining HIPAA compliance. However, practices remain ultimately responsible for ensuring verification accuracy.
Clinical License and Certification Verification
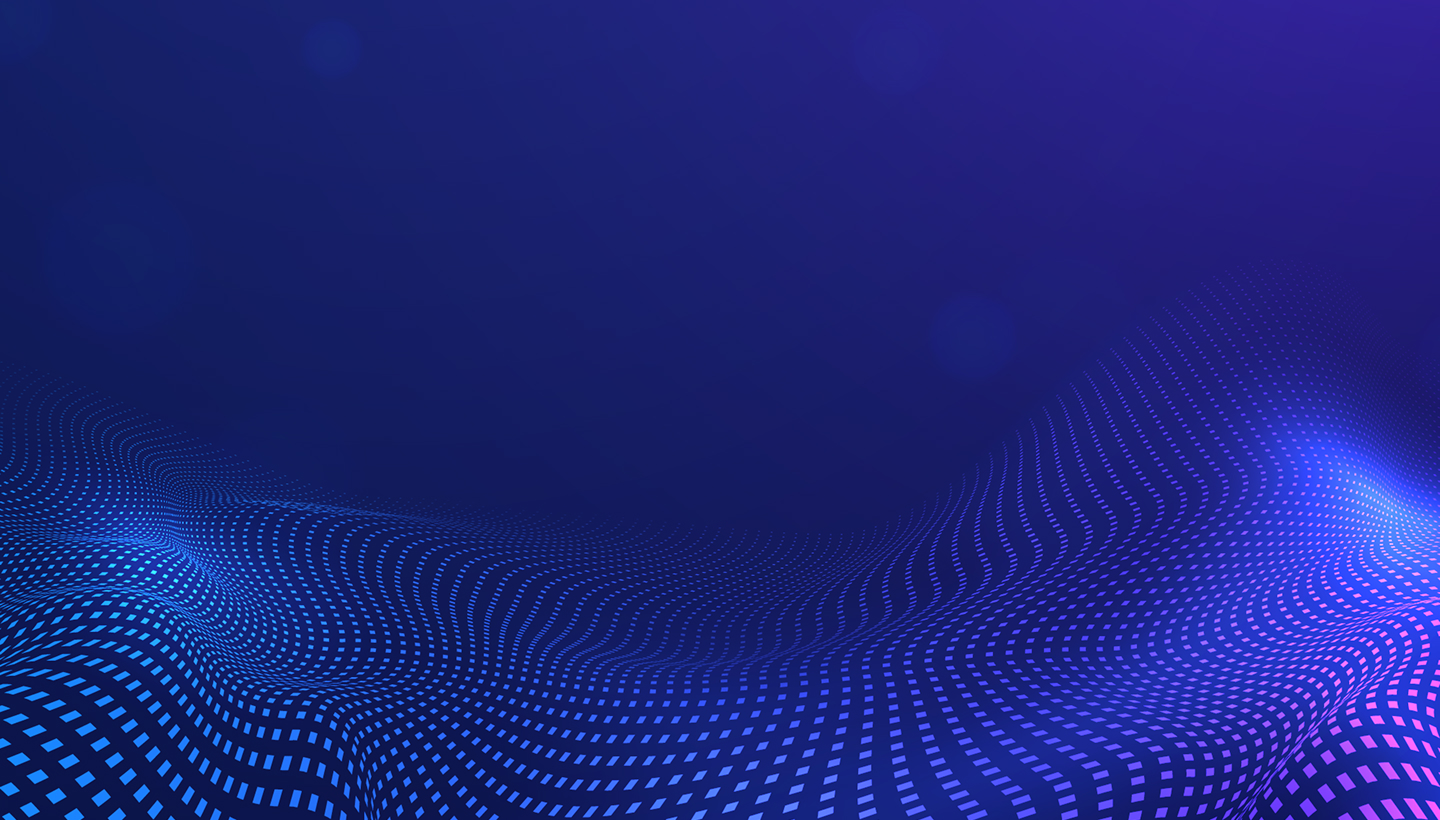
State medical boards, nursing boards, and allied health licensing agencies maintain public databases showing license status and disciplinary actions. Healthcare practices should verify several key elements beyond just confirming a license exists:
- Active, unrestricted license status: Confirms the credential is current and valid for practice
- Issue and expiration dates: Ensures timely renewal and prevents employing individuals with lapsed licenses
- Disciplinary actions or restrictions: Identifies past violations that may disqualify candidates or require additional evaluation
- Scope of practice limitations: Verifies the license permits all duties the position requires
- Board certification verification: Demonstrates advanced competency beyond basic licensure requirements
- DEA registration confirmation: Mandatory for any provider prescribing controlled substances
Board certification verification adds another credibility layer beyond basic licensure. Organizations like the American Board of Medical Specialties and specialty-specific boards maintain verification systems. While board certification may not be legally required, it demonstrates advanced competency and often affects malpractice insurance rates.
Education and Training Verification
Educational verification should confirm degrees from accredited institutions through direct contact with registrar offices or authorized verification services like the National Student Clearinghouse. Diploma mills and fraudulent credentials remain persistent problems in healthcare. Sophisticated fake documents appear authentic without verification. International medical graduates require additional verification through organizations like the Educational Commission for Foreign Medical Graduates (ECFMG).
Clinical training verification includes internships, residencies, fellowships, and specialized certifications. Hospitals and training programs typically provide verification letters confirming dates of participation and successful completion. For physicians, the American Medical Association Physician Masterfile and Federation of State Medical Boards both maintain training history information.
Exclusion List Screening and Ongoing Monitoring
Federal healthcare program exclusion screening represents a mandatory, non-negotiable component of HIPAA compliant employee screening. The Office of Inspector General maintains the List of Excluded Individuals and Entities (LEIE) database containing individuals and organizations barred from participating in Medicare, Medicaid, and other federal healthcare programs. Hiring an excluded individual exposes practices to severe penalties including false claims liability and potential loss of program participation.
The Centers for Medicare & Medicaid Services (CMS) requires screening against exclusion databases before hiring and monthly thereafter throughout employment. This ongoing obligation means practices need systems for regular automated checks rather than one-time verification. The General Services Administration's System for Award Management (SAM) provides another exclusion database that healthcare organizations should check, particularly for administrative and vendor relationships.
| Database | Administered By | Screening Frequency | Purpose |
| OIG LEIE | Office of Inspector General | Before hire + Monthly | Federal healthcare program exclusions |
| SAM Exclusions | General Services Administration | Before hire + Monthly | Government contracting and federal payment exclusions |
| State Medicaid Exclusions | Individual State Agencies | Before hire + Monthly | State-specific program exclusions |
Implementing Exclusion Screening Protocols
Effective exclusion screening requires checking multiple databases because different agencies maintain separate lists. At minimum, healthcare practices should verify candidates against the OIG LEIE, SAM Exclusions database, and state Medicaid exclusion lists. Some states maintain additional healthcare exclusion lists for state-funded programs. Comprehensive screening services often bundle these checks, but practices should verify which databases the service actually searches.
Documentation of exclusion screening is essential for compliance defense. Practices should maintain records showing the date checked, databases searched, individual performing the search, and results for each employee and contractor. Many compliance experts recommend monthly automated screening with documented results retained for at least six years, matching the federal False Claims Act statute of limitations.
Understanding Exclusion Categories and Implications
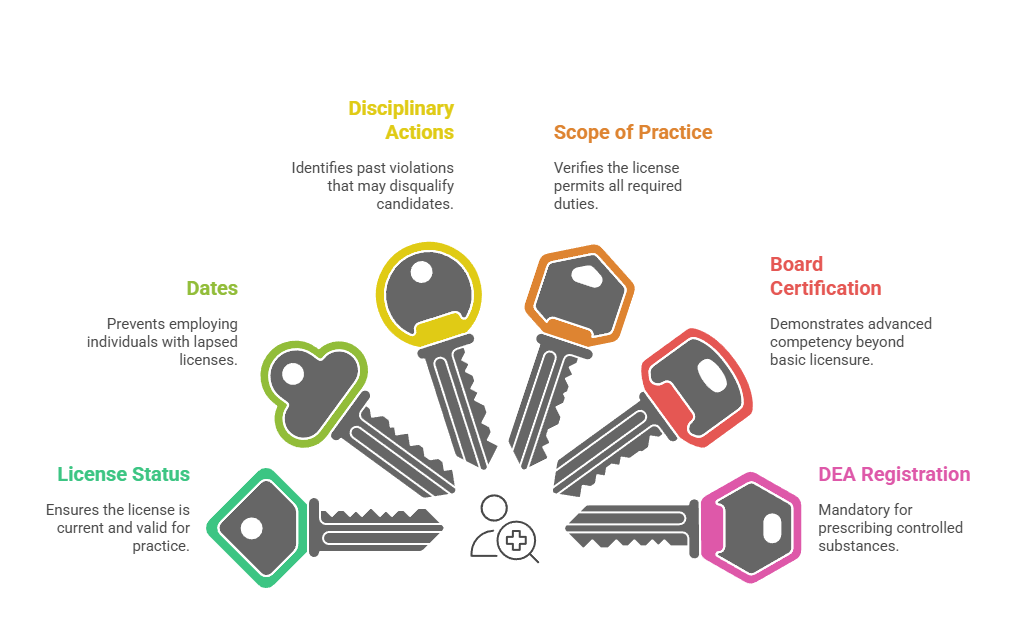
The OIG excludes individuals and entities for various reasons that directly impact their eligibility to participate in federal healthcare programs. Understanding these exclusion categories helps practices assess risk levels and make informed hiring decisions. Healthcare employers must recognize that exclusions carry serious compliance implications.
- Medicare/Medicaid fraud: Billing schemes, false claims, or kickback arrangements that defraud federal programs
- Patient abuse or neglect: Physical, emotional, or financial exploitation of vulnerable individuals in care settings
- Licensing board actions: State medical board sanctions, suspensions, or revocations for serious violations
- Controlled substance convictions: Drug-related offenses involving prescription medications or illegal substances
- Other healthcare-related offenses: Theft from healthcare facilities, embezzlement, or obstruction of investigations
Mandatory exclusions typically last minimum five years and result from specific statutory violations. Permissive exclusions vary in duration based on the severity of conduct. Excluded individuals can apply for reinstatement after their exclusion period expires, but approval isn't automatic and requires demonstrating rehabilitation.
Reference Checks and Employment Verification
Reference checking in healthcare requires more thorough investigation than typical employment verification. While many employers provide only dates of employment and job titles due to liability concerns, healthcare practices need substantive information. This includes clinical competency, patient interaction skills, reliability, and judgment. HIPAA-compliant reference checking balances information gathering with appropriate confidentiality protections.
The National Practitioner Data Bank (NPDB) contains reports of medical malpractice payments, adverse licensure actions, adverse clinical privileges actions, and adverse professional society membership actions. Healthcare organizations have mandatory reporting obligations to the NPDB and can query the database when screening licensed practitioners. NPDB reports provide critical information about competency concerns that candidates may not disclose voluntarily.
Healthcare practices should request multiple professional references including direct supervisors, medical directors, and clinical colleagues who observed the candidate's patient care. References should be contacted by phone rather than relying solely on written letters. This allows for follow-up questions and assessment of reference enthusiasm and hesitation. Key questions should address clinical competency, patient safety incidents, teamwork, professionalism, and whether the reference would rehire the candidate.
Conducting Effective Healthcare Reference Checks
Peer references from other clinicians often provide the most valuable insights for clinical positions. These references can assess technical skills, clinical judgment, and continuing education commitment in ways that administrative supervisors cannot. For physicians and advanced practitioners, hospital credentialing committees and department chairs can provide information about privileges, restrictions, and performance concerns.
Previous employers may be more forthcoming with detailed information when contacted by healthcare compliance officers or medical staff coordinators rather than HR personnel. Healthcare professionals often understand industry-specific concerns and speak a common language that encourages candid discussion. Some practices find success by having their medical director or senior clinician contact the candidate's previous medical director or chief nursing officer directly.
Implementing Compliant Screening Procedures for Small Practices

Small healthcare practices face unique challenges implementing comprehensive HIPAA compliant employee screening with limited administrative resources. Unlike large hospital systems with dedicated credentialing departments, small clinics often rely on office managers or physicians themselves to handle hiring. Creating standardized procedures and leveraging technology solutions makes compliance manageable even with constrained resources.
The key to sustainable compliance in small practices is developing checklists and workflows that ensure consistent application regardless of who conducts screening. Documenting your screening process creates efficiency and compliance protection. This transforms hiring from an ad-hoc scramble into a systematic procedure. These documented processes also satisfy HIPAA Security Rule requirements for workforce security policies and procedures.
Creating Position-Specific Screening Protocols
Different healthcare positions require different screening depths based on patient contact, PHI access, and clinical responsibilities. Small practices should develop three or four screening tiers corresponding to role categories. This approach ensures appropriate verification without unnecessary administrative burden for lower-risk positions:

- High-level clinical positions (physicians, NPs, PAs): Require multi-state criminal checks, DEA/license verification, board certification, NPDB query, exclusion screening, malpractice insurance verification, hospital privileges verification, and thorough reference checks with previous medical directors
- Allied health professionals (RNs, LPNs, medical assistants): Need criminal background checks, license verification, exclusion screening, employment verification, and reference checks emphasizing patient care competency
- Administrative staff with EHR access: Require criminal checks focusing on fraud and theft, exclusion screening, employment verification, and references emphasizing reliability and confidentiality
- Support staff with minimal PHI exposure: Need basic criminal checks, employment verification, and reference checks confirming trustworthiness
Administrative positions with electronic health record access require criminal background checks focusing on fraud and theft. Even non-clinical staff who handle patient information are workforce members under HIPAA, subject to all Privacy and Security Rule requirements. Their screening must address trustworthiness with sensitive information even if they lack medical training.
Utilizing Background Screening Services Effectively
Third-party background screening companies specializing in healthcare can dramatically reduce administrative burden while ensuring compliance. These services typically offer bundled healthcare-specific packages including criminal checks, license verification, exclusion screening, and credential confirmation. When evaluating screening vendors, practices should verify they maintain HIPAA business associate agreements, use secure transmission methods, and provide documentation meeting compliance standards.
Screening service costs vary widely based on package comprehensiveness. Basic criminal background checks start around $30-50 per candidate. Comprehensive healthcare screening packages including credential verification and ongoing monitoring typically range from $150-400 per hire. Though seemingly expensive for small practices, professional screening services cost far less than a single HIPAA violation penalty or negligent hiring lawsuit.
Security Risk Assessment and Access Determination
HIPAA's Security Rule requires covered entities to implement workforce security procedures including authorization, supervision, and termination for individuals accessing electronic protected health information (ePHI). Before granting system access to new employees, practices must conduct security risk assessments determining appropriate access levels. This assessment analyzes what patient information the position requires, which systems and databases need access, and what functions the employee must perform.
For small healthcare practices, formal risk assessment documentation protects against claims that inappropriate access levels contributed to breaches or unauthorized disclosures. This proactive approach prevents over-permissive access assignments that commonly occur when busy practices grant broad system access without careful consideration. The minimum necessary standard requires limiting access to protected health information to the minimum needed for an individual's job function.
During employee screening, practices should evaluate position requirements and establish access profiles before the candidate even begins work. Role-based access control (RBAC) systems align employee access with specific job functions rather than granting individualized custom permissions. Small practices can define four to eight standard role profiles with predetermined access levels. New employees receive the profile matching their position, ensuring consistency and making future audits more manageable.
Training and Acknowledgment Documentation
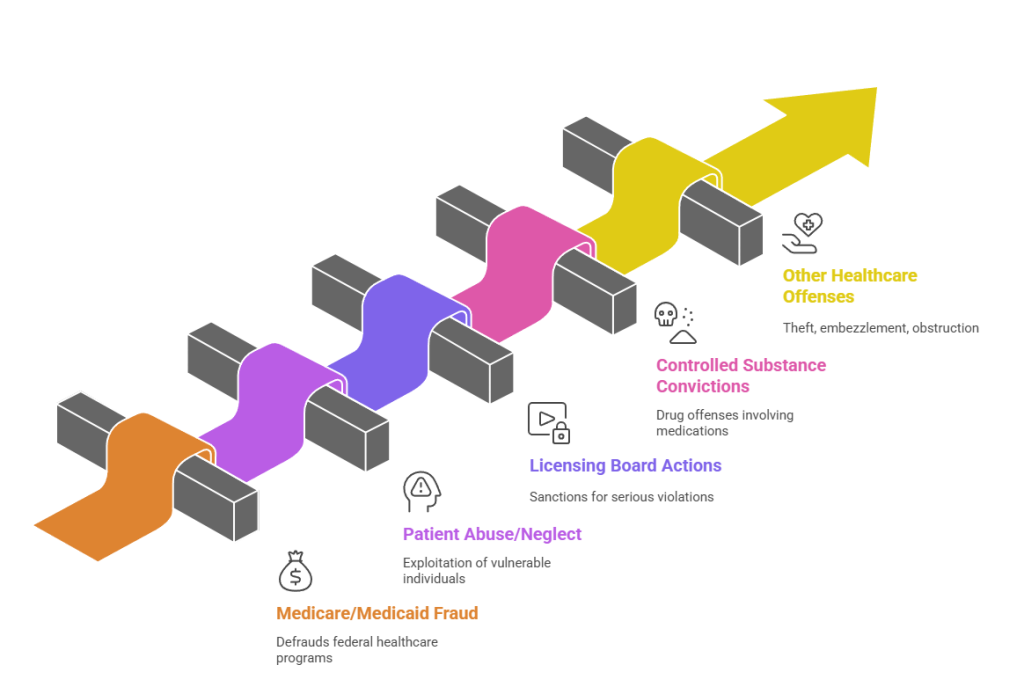
HIPAA training requirements begin before an employee's first day, ensuring workforce members understand their responsibilities from the outset. Comprehensive training programs combined with documented acknowledgments create a foundation for ongoing compliance and establish clear expectations for all staff members handling protected health information.
- Policy acknowledgment during onboarding: Candidates receive and sign privacy notices, security policies, and acceptable use policies before starting work
- Role-specific security training: Employees complete training covering password management, workstation security, email policies, and mobile device requirements before receiving system credentials
- Training documentation maintenance: Completion records become part of employee compliance files, demonstrating workforce security procedure implementation
- Annual retraining requirements: Staff participate in yearly refresher courses addressing emerging threats, recent breaches, and policy updates
- Online training modules: Small practices efficiently deliver HIPAA training through platforms with completion tracking and minimal time away from patient care
Security awareness training specific to the employee's role and access level should occur before system credentials are issued. Documentation of training completion becomes part of the employee's compliance file. This demonstrates workforce security procedure implementation during audits and protects practices from regulatory penalties.
Common Screening Mistakes and Compliance Pitfalls
Even well-intentioned healthcare practices make screening errors that create compliance vulnerabilities and patient safety risks. Understanding common mistakes helps practices avoid expensive lessons from regulatory enforcement or negligent hiring litigation. The Office for Civil Rights and state attorney generals have increased enforcement activity around workforce security failures, making proper screening more critical than ever in 2025.
The most common screening mistake is inconsistent application—thoroughly vetting some candidates while rushing others through abbreviated processes. This inconsistency creates both discrimination liability under employment law and compliance gaps under HIPAA. Every person with PHI access must complete appropriate screening regardless of circumstances.
Many practices conduct comprehensive initial screening but fail to implement ongoing monitoring throughout employment. HIPAA violations, license suspensions, new criminal charges, and exclusion list additions can occur at any point during employment. Monthly automated exclusion screening, annual license verification, and periodic criminal background updates should continue beyond initial hiring.
Documentation Failures
Inadequate screening documentation creates serious compliance risks because healthcare practices bear the burden of demonstrating proper screening occurred. Courts and regulators won't assume compliance—practices must prove it through contemporaneous documentation. Screening files should contain authorization forms, disclosure notices, verification confirmations, database search results, reference notes, and decision rationales.
Practices often make the mistake of having screening documentation scattered across email, paper files, and multiple systems. Centralizing compliance documentation in secure electronic files with access controls ensures availability for audits, investigations, and litigation. Many practice management systems include HR modules for compliance documentation, or practices can use specialized credentialing software.
Conclusion
HIPAA compliant employee screening represents a critical investment in patient safety, regulatory compliance, and practice protection that healthcare organizations cannot afford to overlook. By implementing comprehensive screening procedures including criminal background checks, license verification, credential confirmation, exclusion list monitoring, and thorough reference checks, healthcare practices significantly reduce risks. Small healthcare clinics can achieve compliance through standardized processes, role-based screening tiers, and strategic use of specialized background screening services designed for healthcare's unique requirements. The costs of proper screening pale in comparison to potential penalties for HIPAA violations, negligent hiring liability, and reputational damage from preventable patient safety incidents.
Frequently Asked Questions
HIPAA-compliant employee screening processes can be daunting to navigate, particularly in a medical practice setting where certain considerations come into play. This FAQ portion of the guide tackles the most frequently asked questions that employers typically have, from figuring out what constitutes a HIPAA-compliant employee screening process to factors involving costs, exclusion lists, and document submission.
What makes employee screening HIPAA compliant in healthcare settings?
HIPAA compliant employee screening involves conducting background checks, credential verification, and reference checks through secure channels that protect candidate privacy while gathering information necessary for patient safety. It requires obtaining written authorization before accessing health information, using business associate agreements with screening vendors, and maintaining secure documentation. The process must verify license status, exclusion list standing, and credentials through primary sources while adhering to both HIPAA standards and Fair Credit Reporting Act requirements.
Do small healthcare clinics have the same screening requirements as large hospitals?
Yes, HIPAA compliance obligations apply equally to all covered entities regardless of size, including solo practitioners, small clinics, and large hospital systems. Small healthcare practices must conduct exclusion list screening, license verification, and appropriate background checks for all workforce members with access to protected health information. However, smaller practices can streamline compliance by using third-party screening services, implementing standardized checklists, and developing role-based screening tiers.
How often should healthcare practices screen employees for exclusion lists?
Healthcare practices must screen all employees and contractors against OIG and SAM exclusion databases before hiring and at least monthly throughout employment. CMS requires ongoing monitoring because exclusions can be added at any time, and employing an excluded individual can result in false claims liability. Many practices implement automated monthly screening with documented results rather than manual checks.
Can healthcare employers request medical information during employee screening?
Healthcare employers can conduct medical examinations and request health information only after making a conditional job offer, and only when examinations are job-related under the Americans with Disabilities Act. Pre-employment drug testing is permitted, but results must be treated as confidential medical information with limited access. Employers cannot request complete medical records or require disclosure of all health conditions unrelated to essential job functions.
What criminal background check scope is appropriate for healthcare positions?
Healthcare criminal background checks should cover at minimum seven years and include county, state, and federal criminal records. Relevant offense categories include violent crimes, sexual offenses, fraud, drug-related crimes, theft, and patient abuse. The screening scope should be proportionate to position responsibilities, with direct patient care roles requiring more comprehensive checks than administrative support positions.
Are healthcare practices required to use the National Practitioner Data Bank?
Healthcare organizations including hospitals can query the National Practitioner Data Bank, and hospitals must query when granting clinical privileges. Small clinics and medical practices can access the NPDB only when making credentialing decisions for licensed practitioners who will have clinical privileges. However, many compliance experts recommend NPDB queries for physicians and advanced practitioners even in small practice settings when permissible.
How can small practices manage screening costs effectively?
Small healthcare practices can manage screening costs by developing risk-based screening tiers with comprehensive checks for high-risk clinical positions and more focused screening for lower-risk roles. Negotiating volume discounts with screening vendors, using practice management software with HR modules, and implementing reusable checklists increases efficiency. Many screening services offer healthcare-specific packages ranging from $150-400 per hire.
What happens if a current employee appears on an exclusion list?
If a current employee appears on a federal exclusion list, the practice must immediately prevent that individual from providing any services related to federal healthcare program beneficiaries. This typically requires immediate termination or reassignment to roles involving exclusively private-pay patients if such positions exist. The practice should document the discovery, immediate actions taken, and review claims submitted involving the excluded individual's services.
Additional Resources
- HHS Office for Civil Rights - HIPAA for Professionals
https://www.hhs.gov/hipaa/for-professionals/index.html - Office of Inspector General - List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/index.asp - National Practitioner Data Bank - Healthcare Integrity and Protection Data Bank
https://www.npdb.hrsa.gov - Federal Trade Commission - Using Consumer Reports for Employment Purposes
https://www.ftc.gov/business-guidance/resources/using-consumer-reports-employment-purposes - CMS Medicare Learning Network - Screening Requirements
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/index.html - System for Award Management (SAM) Exclusions Database
https://sam.gov/content/exclusions

GCheck Editorial Team
Meet the GCheck Editorial Team, your trusted source for insightful and up-to-date information in the world of employment background checks. Committed to delivering the latest trends, best practices, and industry insights, our team is dedicated to keeping you informed.
With a passion for ensuring accuracy, compliance, and efficiency in background screening, we are your go-to experts in the field. Stay tuned for our comprehensive articles, guides, and analysis, designed to empower businesses and individuals with the knowledge they need to make informed decisions.
At GCheck, we're here to guide you through the complexities of background checks, every step of the way.