Tennessee healthcare facilities must comply with both state Department of Health regulations and federal CMS requirements when conducting background checks on healthcare workers. These requirements include criminal history screenings, abuse registry searches, and employment verification. Understanding Tennessee healthcare background check requirements is essential for employers to maintain compliance and ensure patient safety while avoiding costly penalties.
Key Takeaways
- Tennessee healthcare facilities must conduct comprehensive background checks including FBI fingerprinting, state criminal records, and OIG exclusion list screenings for all direct patient care workers.
- The Tennessee Department of Health requires healthcare employers to check both state and federal abuse registries before hiring healthcare workers.
- CMS background check requirements in Tennessee mandate screening for all long-term care facility employees at least every five years.
- Healthcare facilities face penalties up to $25,000 per violation for failing to conduct required background screenings on employees.
- Certain criminal convictions create automatic disqualifications for healthcare employment in Tennessee, including violent felonies and abuse-related offenses.
- Tennessee health facility background check rules require continuous monitoring of employees through the OIG exclusion list and state licensure databases.
Understanding Tennessee Healthcare Background Check Requirements

Tennessee healthcare background check requirements represent a complex framework combining state regulations and federal mandates. The Tennessee Department of Health establishes baseline screening standards for healthcare facilities. Meanwhile, CMS imposes additional requirements for Medicare and Medicaid-certified organizations. Healthcare employers must navigate both regulatory systems to ensure full compliance and protect patient safety.
Tennessee strengthened its background check laws in 2019 following patient safety concerns. Today's requirements reflect a comprehensive risk management strategy addressing criminal history, professional misconduct, and abuse allegations. State surveyors regularly audit background check procedures during facility inspections. Violations can result in substantial fines, license restrictions, or facility closure.
Tennessee Department of Health Background Check Mandates
The Tennessee Department of Health requires licensed healthcare facilities to conduct thorough background screenings before allowing employees to provide direct patient care. These mandates apply to hospitals, nursing homes, assisted living facilities, home health agencies, and ambulatory surgical centers. State regulations establish minimum screening components including verification of professional licenses, searches of state criminal databases, and checks against abuse registries. Employers cannot permit workers to begin patient care activities until completing all mandatory screening elements.
Healthcare facilities must document all screening activities and maintain records for inspection by health department surveyors. They must also implement ongoing monitoring systems to detect disqualifying events after initial employment. This vigilance helps organizations identify compliance issues before they result in patient harm or regulatory citations.
Criminal History Screening Components
Tennessee healthcare employers must conduct comprehensive criminal background checks that include both state and federal-level searches. The Tennessee Bureau of Investigation (TBI) processes fingerprint-based criminal history checks for healthcare workers. FBI fingerprinting provides national-level criminal history information capturing offenses committed outside Tennessee's borders. The criminal screening process typically takes 2-4 weeks for completion.
New hires cannot provide direct patient care until the facility receives cleared background check results. Healthcare organizations must evaluate criminal history information according to Tennessee's disqualification standards. The following criminal convictions create automatic employment barriers in healthcare settings:
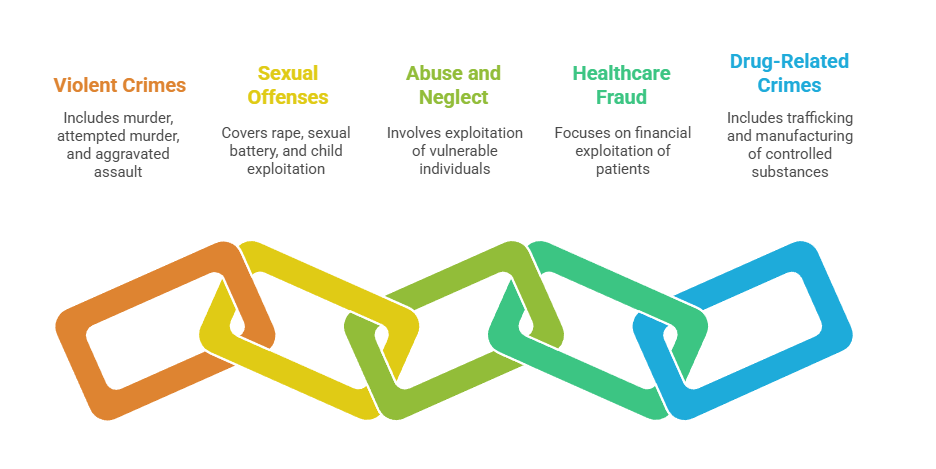
- Murder, attempted murder, or voluntary manslaughter
- Aggravated assault, aggravated robbery, or kidnapping
- Sexual offenses including rape, sexual battery, or child exploitation
- Abuse, neglect, or exploitation of vulnerable adults or children
- Healthcare fraud or financial exploitation of patients
- Drug trafficking or manufacturing controlled substances
Facilities maintain discretion to deny employment based on other criminal convictions that may demonstrate unfitness for patient care responsibilities. Employers must document their decision-making process when evaluating criminal history to demonstrate compliance with fair hiring practices and FCRA requirements.
Registry and Exclusion List Searches
Tennessee healthcare facilities must search multiple state and federal registries before hiring healthcare workers. The Tennessee Department of Health maintains an abuse registry documenting substantiated cases of abuse, neglect, or misappropriation involving vulnerable populations. Healthcare employers must verify that applicants do not appear on this registry before allowing patient contact.
Federal exclusion lists represent critical screening components for facilities participating in Medicare or Medicaid programs. CMS background check requirements in Tennessee mandate monthly searches of the OIG List of Excluded Individuals and Entities (LEIE) and the System for Award Management (SAM) exclusion database. Employing excluded individuals can result in severe financial penalties and loss of Medicare/Medicaid participation.
| Registry Type | Administering Agency | Search Frequency | Scope |
| State Abuse Registry | Tennessee Department of Health | Pre-employment & Annual | Abuse/neglect findings in Tennessee |
| OIG LEIE | U.S. Department of Health & Human Services | Monthly | Federal healthcare program exclusions |
| SAM Exclusions | General Services Administration | Monthly | Government contracting exclusions |
| State Medicaid Exclusions | TennCare | Monthly | Tennessee Medicaid terminations |
Healthcare organizations must establish documented procedures for conducting registry searches and responding to positive matches. Monthly screening helps facilities identify employees who become excluded after initial hiring.
CMS Background Check Requirements in Tennessee
Long-term care facilities in Tennessee must comply with federal CMS background check requirements established under Section 6201 of the Affordable Care Act. These regulations apply to nursing homes, skilled nursing facilities, and intermediate care facilities participating in Medicare or Medicaid programs. CMS mandates comprehensive background screening for all employees, contractors, and volunteers with direct access to residents or resident property.
The CMS framework requires both pre-employment screening and periodic rescreening every five years. Tennessee implemented these requirements through its long-term care licensure regulations. Facilities must conduct fingerprint-based criminal background checks, state abuse registry searches, and federal exclusion list screenings. The following screening elements comprise mandatory CMS background check components:

- FBI fingerprint-based criminal history check
- State criminal background check through Tennessee Bureau of Investigation
- Tennessee abuse registry search
- OIG LEIE and SAM exclusion list verification
- Employment history verification for previous seven years
- Professional license verification and disciplinary action search
Facilities must complete initial screening before granting access to residents or resident property. Provisional employment may be permitted during background check processing under direct supervision with documented risk mitigation measures. Regulatory surveys by CMS scrutinize background check procedures, with deficiencies potentially resulting in civil monetary penalties.
CMS Provisional Employment Guidelines
The Centers for Medicare & Medicaid Services permits limited provisional employment while awaiting final background check results under specific conditions. Direct supervision by cleared staff members must be provided during all resident interactions. Most facilities limit provisional periods to 30 days or less. Immediate termination of provisional employees is required if preliminary screening reveals disqualifying information.
CMS Penalty Structure for Non-Compliance
CMS imposes significant financial penalties on facilities that fail to conduct required background checks. Civil monetary penalties can range from $1,000 to $10,000 per day of non-compliance. Facilities may also face termination from Medicare and Medicaid participation for serious or repeated violations.
Professional License and Credential Verification
Tennessee medical facility employment screening must include verification of professional licenses and credentials for all licensed healthcare workers. The Tennessee Department of Health maintains online verification systems for nurses, physicians, pharmacists, and allied health professionals. Employers must confirm active licensure status and investigate any disciplinary actions before finalizing employment offers.
Credential verification extends beyond basic licensure to include specialty certifications, educational qualifications, and professional training. Healthcare facilities should verify credentials directly with issuing organizations rather than relying solely on applicant-provided documentation. The National Practitioner Data Bank (NPDB) provides additional information about malpractice payments and adverse actions for physicians, dentists, and other practitioners. Tennessee requires healthcare employers to establish systems for continuous monitoring of employee licensure status.
Employment and Education Verification Requirements
Comprehensive Tennessee healthcare worker screening requirements include verification of previous employment and educational credentials. Healthcare facilities should contact previous employers to confirm employment dates, positions held, and eligibility for rehire. This verification process helps identify performance concerns or patient care issues that may not appear in criminal background checks.
Education verification confirms that healthcare workers possess required degrees, diplomas, or training certificates. Employers should request official transcripts directly from educational institutions. For foreign-educated healthcare workers, credential evaluation services can verify educational equivalency to U.S. standards.
| Verification Type | Information to Confirm | Timeframe |
| Employment History | Dates, titles, responsibilities, rehire eligibility | Previous 7 years |
| Education | Degrees, graduation dates, accreditation status | All claimed credentials |
| Professional Training | Certifications, continuing education, specialized skills | Current certifications |
Healthcare organizations should develop standardized verification procedures that document all confirmation attempts. Thorough verification reduces the risk of hiring individuals who have misrepresented qualifications or concealed problematic employment histories.
Disqualifying Offenses and Hiring Restrictions
Tennessee law establishes specific criminal offenses that automatically disqualify individuals from healthcare employment. These mandatory exclusions protect vulnerable populations from individuals who have demonstrated dangerous behaviors or violated trust relationships. Healthcare facilities cannot employ individuals with disqualifying convictions in positions involving direct patient care, regardless of time elapsed or rehabilitation efforts.
Beyond automatic disqualifications, facilities should consider additional factors when evaluating criminal history. Tennessee follows a risk-based approach that examines offense nature, recency, frequency, and relationship to job responsibilities. The following factors should guide hiring decisions involving criminal history:
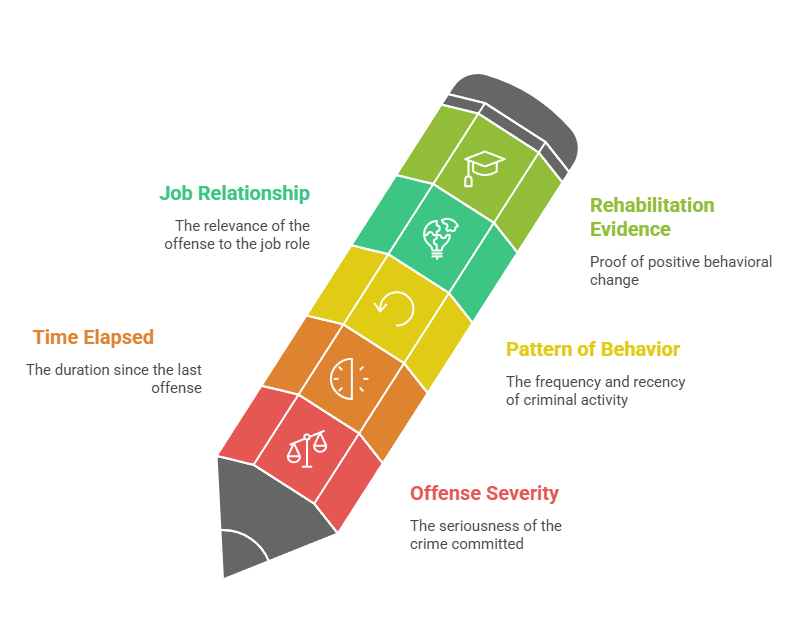
- Offense Severity: Violent felonies and crimes against persons pose higher patient safety risks than property offenses.
- Time Elapsed: Convictions occurring many years ago with no subsequent criminal activity suggest successful rehabilitation.
- Pattern of Behavior: Multiple convictions or recent criminal activity indicates ongoing risk concerns that may justify employment denial.
- Job Relationship: Convictions directly related to healthcare responsibilities warrant greater scrutiny than unrelated offenses.
- Rehabilitation Evidence: Completion of treatment programs, educational advancement, and stable employment history demonstrate positive behavioral change.
Healthcare facilities should document their evaluation process and maintain consistent decision-making standards. Employers should consult legal counsel when evaluating complex criminal history situations to ensure compliance with anti-discrimination laws.
Background Check Procedures and Timelines
Healthcare facilities must establish systematic background check procedures that ensure consistent compliance with Tennessee healthcare background check requirements. The screening process begins when applicants accept conditional employment offers and sign authorization forms. Tennessee healthcare employers typically follow a sequential screening approach that prioritizes time-sensitive verifications. License verification and OIG exclusion searches occur first since these provide immediate results.
The background check timeline involves these key stages:
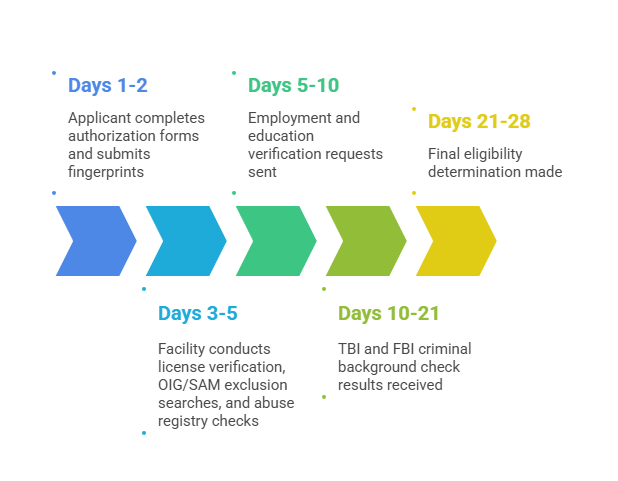
- Days 1-2: Applicant completes authorization forms and submits fingerprints
- Days 3-5: Facility conducts license verification, OIG/SAM exclusion searches, and abuse registry checks
- Days 5-10: Employment and education verification requests sent
- Days 10-21: TBI and FBI criminal background check results received
- Days 21-28: Final eligibility determination made
Healthcare facilities should establish clear communication protocols for updating applicants on screening status. Proactive communication helps maintain candidate engagement while demonstrating organizational professionalism.
Compliance Documentation and Record Retention
Tennessee health facility background check rules require comprehensive documentation of all screening activities and hiring decisions. Healthcare employers must maintain records demonstrating compliance with state and federal background check requirements. These records serve as evidence during licensing surveys, CMS inspections, and potential legal challenges to employment decisions.
Required documentation includes background check authorization forms, screening results from all required sources, and written evaluations of any adverse findings. Facilities must document the decision-making process when criminal history or other concerns emerge during screening. Record retention requirements vary based on regulatory framework and employment outcome.
| Document Type | Retention Period | Storage Requirements |
| Background check authorizations | Duration of employment + 7 years | Secure, confidential files |
| Criminal history reports | Duration of employment + 7 years | Limited access, encrypted if electronic |
| Registry search results | Duration of employment + 3 years | Documented monthly searches |
| Employment verification | Duration of employment + 7 years | Secure personnel files |
| Adverse action notices | 5 years from action date | FCRA compliance files |
Healthcare organizations should implement secure storage systems that protect confidential background check information from unauthorized access. Regular audits of background check files help identify documentation gaps and ensure compliance with retention requirements.
Ongoing Monitoring and Rescreening Requirements
Tennessee healthcare facilities must implement continuous monitoring systems that detect changes in employee eligibility after initial hiring. CMS background check requirements in Tennessee mandate rescreening every five years for long-term care facility employees. Beyond mandatory rescreening, facilities should conduct monthly OIG exclusion list searches and annual license verification for all healthcare workers.
Effective ongoing monitoring programs include these essential components:
- Monthly Exclusion List Screening: Automated systems check OIG LEIE, SAM, and state Medicaid exclusion databases monthly for all employees, contractors, and volunteers.
- Annual License Verification: Healthcare facilities should verify professional licenses annually to confirm active status and identify disciplinary actions.
- Criminal History Alerts: Some background screening providers offer continuous monitoring services that notify employers when employees are arrested or convicted of new offenses.
- Incident Reporting Systems: Facilities should require employees to self-report arrests, license actions, or exclusions that occur during employment.
Healthcare organizations must establish documented procedures for responding to adverse findings discovered through ongoing monitoring. Immediate suspension may be necessary when employees appear on exclusion lists or face license revocations.
Background Check Costs and Fee Structures
Healthcare employers in Tennessee typically bear the costs associated with conducting required background checks. Criminal history checks through the Tennessee Bureau of Investigation cost approximately $29 for fingerprint processing. FBI fingerprinting adds another $13.25 for federal criminal history searches. Total screening costs per applicant range from $100 to $250 depending on the comprehensiveness of verification services.
Third-party background screening vendors offer comprehensive packages that bundle multiple verification components at discounted rates. These vendors typically charge $75-150 per screening including criminal history, license verification, employment verification, and exclusion list searches.
State vs. Federal Requirement Differences
Tennessee healthcare background check requirements reflect both state Department of Health regulations and federal CMS mandates. While these frameworks overlap significantly, important differences exist in scope, frequency, and disqualification standards. Healthcare facilities must comply with the most stringent requirements when state and federal rules diverge.
Key differences between state and federal requirements include:
- Rescreening Frequency: CMS mandates five-year rescreening for long-term care workers; Tennessee state law does not specify mandatory rescreening intervals for other healthcare settings
- Provisional Employment: Federal regulations permit provisional employment during background check processing; Tennessee rules vary by facility type
- Disqualifying Offenses: State law establishes automatic disqualifications; CMS requires individualized assessment of criminal history
- Scope of Workers: CMS covers all individuals with resident access in long-term care; state requirements focus primarily on direct patient care workers
Healthcare organizations should conduct comprehensive analyses identifying all applicable requirements based on facility type and program participation.
Special Considerations for Different Healthcare Settings
Tennessee healthcare background check requirements vary somewhat based on facility type and patient population served. Long-term care facilities face the most stringent background check requirements due to vulnerable resident populations and federal CMS oversight. Hospitals and acute care facilities follow Tennessee Department of Health regulations requiring background checks for clinical staff.
Hospital Background Check Requirements
Hospitals must screen physicians, nurses, therapists, and support staff providing patient care services. Hospital background check programs should address both employed workers and medical staff members with privileges. Hospitals should also conduct background checks on contract workers and temporary staff provided by staffing agencies.
Home Health Agency Screening Challenges
Home health agencies face unique challenges conducting background checks on workers who provide services in patients' homes. These agencies must ensure comprehensive screening before allowing home visits since workers operate with minimal supervision in intimate settings. Tennessee requires home health agencies to conduct abuse registry checks and criminal background screenings for all direct care workers.
Ambulatory Surgery Center Considerations
Ambulatory surgery centers must conduct background checks on surgical staff, nurses, and support personnel involved in patient care. Tennessee requires surgery centers to verify professional licenses and conduct criminal background checks for all clinical staff. Surgery centers should pay particular attention to drug-related criminal history when evaluating applicants due to controlled substance access.
FCRA Compliance in Healthcare Background Screening
The Fair Credit Reporting Act (FCRA) establishes federal requirements that Tennessee healthcare employers must follow when conducting background checks through third-party screening companies. FCRA protects applicant rights by requiring clear disclosures, written authorization, and adverse action procedures.
Healthcare employers must provide standalone written disclosure explaining that background checks will be conducted before obtaining applicant authorization. When background checks reveal information that may result in adverse employment decisions, facilities must follow FCRA's pre-adverse action process. Employers must provide applicants with copies of background check reports and summaries of FCRA rights before taking adverse action.
FCRA compliance requirements for Tennessee healthcare employers include:
- Clear Authorization: Obtain written permission on standalone disclosure forms before conducting background checks through third-party screening companies.
- Adverse Action Notice: Provide pre-adverse action notice including background check copy and FCRA rights summary before making final decisions based on screening results.
- Dispute Procedures: Establish processes for applicants to challenge inaccurate background check information and delay adverse action pending dispute resolution.
- Information Security: Implement safeguards protecting confidential background check information from unauthorized access or disclosure.
- Certification Compliance: Ensure background screening vendors certify compliance with FCRA requirements and permissible purpose standards.
Healthcare facilities should train hiring managers on FCRA compliance procedures and establish workflows that build in required notification periods.
Common Compliance Mistakes and How to Avoid Them
Tennessee healthcare facilities frequently encounter compliance challenges when implementing background check programs. Understanding common mistakes helps organizations develop preventive controls and avoid regulatory violations. One frequent error involves incomplete screening that omits required registry searches or verification components. Comprehensive screening checklists ensure staff complete all mandatory components before employment authorization.
Another common mistake occurs when facilities allow workers to begin patient care before receiving cleared background check results. Allowing unsupervised patient contact before screening completion violates Tennessee healthcare background check requirements and creates significant liability exposure. Healthcare employers also face challenges documenting screening decisions and maintaining required records.
Additional compliance pitfalls include:
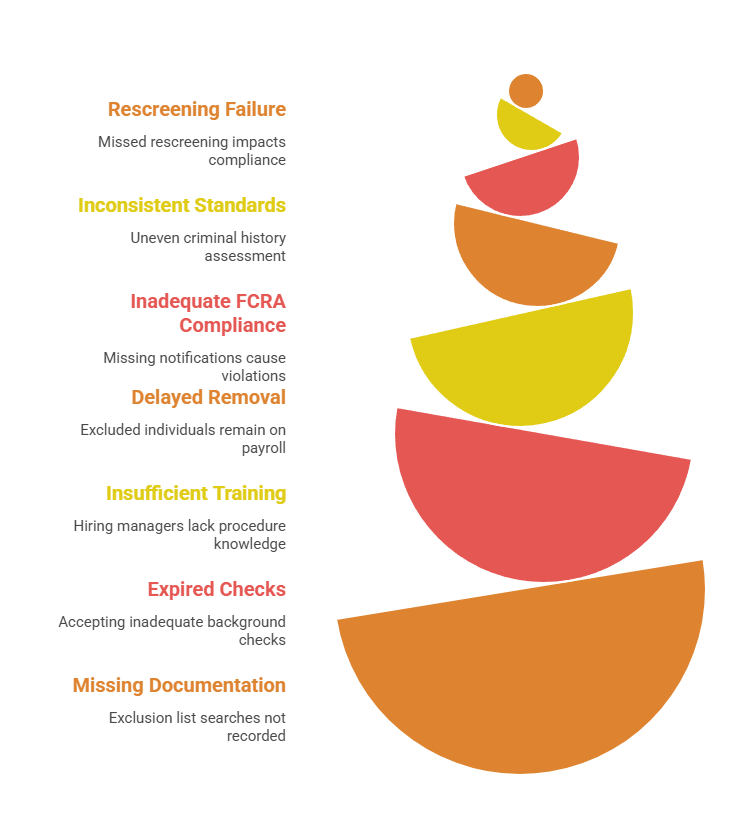
- Failing to conduct required rescreening at specified intervals for long-term care employees
- Inconsistent application of hiring standards when evaluating criminal history across applicants
- Inadequate FCRA compliance including missing pre-adverse action notifications
- Delayed removal of excluded individuals from payroll after appearing on OIG lists
- Insufficient training of hiring managers on background check procedures
- Accepting expired or inadequate background checks from staffing agencies
- Missing documentation of monthly OIG exclusion list searches
Healthcare facilities should establish robust compliance programs with clear policies, standardized procedures, staff training, and regular monitoring.
Implementation Best Practices for Healthcare Employers
Successfully implementing Tennessee healthcare background check requirements demands systematic planning and organizational commitment. Healthcare facilities should begin by conducting comprehensive assessments of current screening practices. Developing written policies and procedures is essential for ensuring consistent screening across hiring decisions and facility locations.
The following best practices support effective background check programs:
- Standardized Forms and Checklists: Develop templates for authorization forms, screening checklists, and evaluation documentation that ensure consistent processes.
- Vendor Selection Criteria: Choose background screening vendors based on accuracy, compliance support, turnaround time, and customer service quality.
- Applicant Communication Protocols: Establish clear communication practices that keep candidates informed throughout the screening process.
- Provisional Employment Guidelines: Create specific criteria for when provisional employment is appropriate and what supervision is required.
- Quality Assurance Audits: Conduct quarterly audits of random background check files to verify documentation completeness.
- Legal Review Processes: Establish procedures for consulting employment counsel on complex criminal history evaluations or FCRA compliance questions.
- Continuous Improvement Mindset: Regularly evaluate screening metrics like turnaround time and documentation deficiencies to identify improvement opportunities.
Healthcare facilities should designate specific staff members responsible for background check program oversight. Clear accountability improves compliance and prevents screening delays.
Conclusion
Tennessee healthcare background check requirements protect patients by ensuring healthcare workers meet safety and competency standards established by state and federal regulators. Healthcare facilities must navigate complex regulations from the Tennessee Department of Health and CMS while maintaining FCRA compliance. Comprehensive screening programs combining criminal background checks, registry searches, credential verification, and ongoing monitoring help organizations meet these obligations. By implementing systematic procedures, maintaining thorough documentation, and providing regular staff training, Tennessee healthcare employers can build compliant background check programs that support quality patient care and organizational integrity.
Frequently Asked Questions
What background checks are required for Tennessee healthcare workers?
Tennessee requires healthcare workers to complete FBI fingerprint-based criminal background checks, Tennessee Bureau of Investigation criminal history searches, state abuse registry checks, and federal OIG exclusion list verification. Healthcare facilities must also verify professional licenses, employment history, and educational credentials for all direct patient care workers before allowing them to begin duties.
How long do Tennessee healthcare background checks take to complete?
Tennessee healthcare background checks typically take 2-4 weeks to complete from fingerprint submission through final results receipt. License verification and OIG exclusion list searches provide immediate results. However, criminal history checks through TBI and FBI require 10-21 days for processing.
How much do healthcare background checks cost in Tennessee?
Healthcare background checks in Tennessee cost between $100-250 per applicant depending on screening components. TBI fingerprint processing costs approximately $29. FBI criminal history checks add $13.25. Third-party screening vendors charge $75-150 for comprehensive packages including verification services.
Can Tennessee healthcare workers start working before background checks are complete?
Tennessee regulations permit provisional employment in some healthcare settings while awaiting background check results. However, facilities must implement direct supervision and document risk assessments. Facilities must complete abuse registry and OIG exclusion list searches before allowing any patient contact. Most facilities limit provisional periods to 30 days or less.
What disqualifies someone from healthcare employment in Tennessee?
Tennessee automatically disqualifies individuals convicted of murder, sexual offenses, patient abuse, healthcare fraud, kidnapping, aggravated assault, or exploitation of vulnerable adults from healthcare employment. Additional convictions may create discretionary disqualifications based on offense severity, recency, and relationship to job responsibilities.
How often must Tennessee healthcare facilities rescreen employees?
CMS requires long-term care facilities in Tennessee to conduct comprehensive background rescreening every five years for all employees with resident access. Other healthcare facilities should implement ongoing monitoring including monthly OIG exclusion list searches and annual license verification. Many hospitals and clinics conduct criminal rescreening every 3-5 years as a best practice.
Do volunteers in Tennessee healthcare facilities need background checks?
Yes, volunteers in Tennessee healthcare facilities who have direct patient contact or access to patient information must complete the same background check requirements as paid employees. This includes criminal history checks, abuse registry searches, and OIG exclusion list verification.
What is the Tennessee abuse registry and how do employers check it?
The Tennessee abuse registry is a state database maintained by the Department of Health containing substantiated findings of abuse, neglect, or misappropriation involving vulnerable adults and children. Healthcare employers must search this registry before hiring workers who will have patient contact. Registry searches can be conducted through the Tennessee Department of Health's online verification system or through approved background screening vendors.
Additional Resources
- Tennessee Department of Health Healthcare Facility Licensing
https://www.tn.gov/health/health-program-areas/health-professional-boards/facility-licensure.html - CMS Background Checks for Long-Term Care Facilities
https://www.cms.gov/medicare/provider-enrollment-and-certification/surveycertificationgeninfo/background-checks-long-term-care-facilities - OIG List of Excluded Individuals and Entities
https://oig.hhs.gov/exclusions/ - Tennessee Bureau of Investigation Background Check Services
https://www.tn.gov/tbi/criminal-history-information.html - Federal Trade Commission FCRA Guidance for Employers
https://www.ftc.gov/business-guidance/resources/using-consumer-reports-what-employers-need-know - National Practitioner Data Bank
https://www.npdb.hrsa.gov/ - Tennessee Healthcare Association Compliance Resources
https://tnhealthcare.org/
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub

How Long Does a Background Check Take? A Complete 2025 Guide
13 Dec, 2023 • 14 min read
The Ultimate Background Check Guide
13 Dec, 2023 • 4 min read
The Ultimate Guide to Employment Background Checks
13 Dec, 2023 • 10 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.

