Indiana healthcare facilities face expanded criminal history screening requirements under recent ISDH regulatory updates, mandating comprehensive background checks for all direct patient care workers and increasing scrutiny of disqualifying offenses. Healthcare administrators must implement enhanced screening protocols by specified compliance deadlines to avoid regulatory penalties ranging from $1,000 to $25,000 per violation while protecting their organizations from patient safety liability exposure.
Key Takeaways
- Indiana healthcare facilities must conduct expanded criminal history checks for all employees with direct patient care access, including clinical staff, nursing assistants, and support personnel working in patient areas.
- ISDH regulations now require national fingerprint-based FBI background checks in addition to state-level screening, with results processed through the Indiana State Police and cross-referenced against healthcare exclusion databases.
- Disqualifying offenses include violent crimes, sexual offenses, drug-related felonies, patient abuse convictions, and theft crimes committed within specified lookback periods that vary by offense severity.
- Healthcare employers must complete background check verification before an employee's first day of patient contact, with provisional employment prohibited during the screening process for positions involving vulnerable populations.
- The lookback period for criminal history evaluation extends 7 years for most felonies and indefinitely for specified violent and sexual offenses, with state-specific rehabilitation consideration requirements.
- Failure to maintain compliant background check documentation exposes healthcare organizations to ISDH enforcement actions, federal funding jeopardy, and increased civil liability in patient safety litigation.
- Healthcare administrators should establish standardized screening workflows incorporating conditional offer protocols, disclosure requirements, FCRA-compliant adverse action procedures, and secure record retention systems meeting 7-year documentation requirements.
Understanding Indiana's Expanded Healthcare Background Check Framework
The Indiana State Department of Health (ISDH) implemented comprehensive regulatory expansions in 2024 that fundamentally altered background check requirements for healthcare workers across all facility types. These changes respond to federal CMS guidance, patient safety incident data analysis, and coordination with the Office of Medicaid Policy and Planning to standardize screening protocols statewide. The new framework addresses previous compliance gaps that allowed varying standards across different healthcare settings.
Indiana Code 16-27-2 grants ISDH broad authority to establish and enforce background check requirements for healthcare facility employees, contractors, and volunteers. The 2024 regulatory expansion builds upon existing statutes by incorporating 410 IAC 16.2-5 standards previously limited to long-term care facilities. Healthcare administrators must recognize these requirements carry statutory force with enforcement mechanisms including facility licensing sanctions and civil monetary penalties.
Covered Facilities and Employee Categories
The 2025 requirements apply to all Indiana healthcare facilities operating under ISDH licensure. This includes general hospitals, critical access hospitals, specialty hospitals, ambulatory surgical centers, community mental health centers, hospice programs, home health agencies, and outpatient clinical facilities. Previous exemptions for certain outpatient settings and physician-owned practices with fewer than 10 employees have been eliminated under the standardized approach.
Covered employee categories extend beyond licensed clinical professionals to encompass any individual with potential unsupervised patient access. Healthcare facilities must screen the following positions:

- Direct Care Providers: Registered nurses, licensed practical nurses, certified nursing assistants, medical assistants, and patient care technicians providing hands-on patient services
- Clinical Support Staff: Laboratory phlebotomists, respiratory therapy assistants, radiology technicians, and physical therapy aides with regular patient contact
- Patient Services Personnel: Dietary staff entering patient areas, environmental services personnel cleaning patient rooms, patient transporters, and unit clerks
- Administrative Staff: Personnel with routine access to patient care floors, medical records departments, or areas where patients receive treatment
Contract employees, temporary agency staff, and volunteer positions with patient contact require identical screening despite their non-permanent status. Healthcare facilities remain responsible for ensuring third-party contractors maintain compliant screening documentation.
Required Components of Compliant Background Checks
A compliant Indiana healthcare background check comprises multiple screening elements that must be completed, documented, and evaluated according to ISDH specifications. Healthcare employers cannot substitute partial screening or rely exclusively on self-disclosure to meet regulatory requirements. Each component serves a distinct purpose in comprehensive risk assessment.
State and Federal Criminal History Searches
The Indiana State Police Criminal History Repository search forms the foundation of compliant screening. It provides access to conviction records, pending charges, and arrest data from all 92 Indiana counties. Healthcare facilities must submit fingerprint-based searches through approved channeling agencies rather than name-based searches, which fail to meet ISDH standards due to accuracy limitations.
The expanded ISDH requirements mandate FBI national criminal history searches for all covered positions. This federal search queries the Interstate Identification Index (III), capturing criminal records from all 50 states, U.S. territories, and federal prosecution databases. Healthcare facilities must use approved fingerprinting services registered with both the Indiana State Police and FBI, with electronic submission strongly preferred over traditional ink card methods.
Processing times vary based on submission method and existing records. State background checks typically return within 5-7 business days for Indiana residents. FBI searches range from 24 hours to 14 days depending on whether fingerprints match existing records. Healthcare administrators should allow 10-15 business days for complete results.
Healthcare Exclusion Database Verification
Compliant screening extends beyond criminal history to include mandatory searches of healthcare exclusion databases maintained by federal and state agencies. These databases identify providers barred from federal healthcare programs due to fraud, patient abuse, or license revocations. Healthcare facilities must search the following databases:
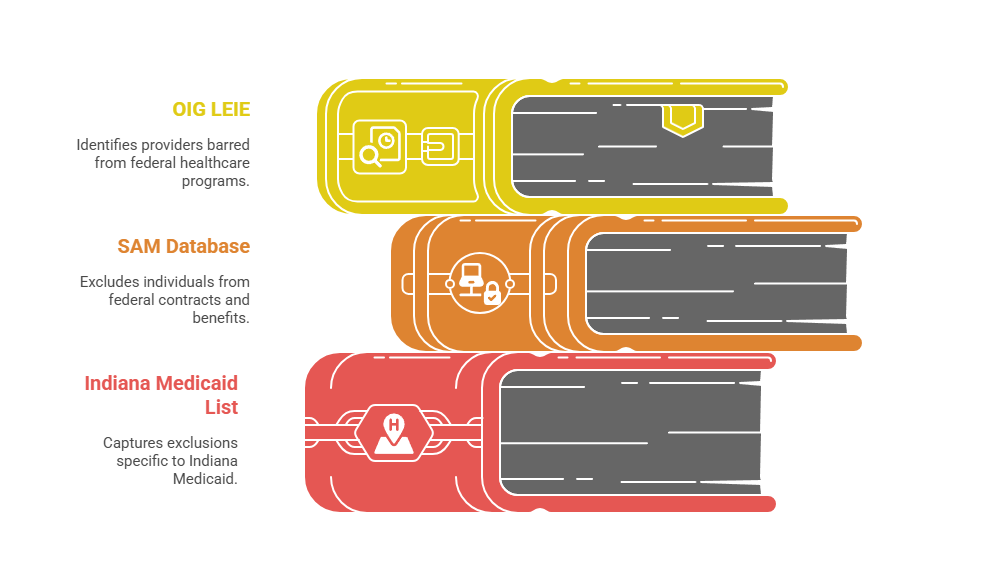
- OIG LEIE: The HHS Office of Inspector General's List of Excluded Individuals and Entities identifies providers barred from Medicare, Medicaid, and all federal healthcare programs.
- SAM Database: The System for Award Management excludes individuals from federal contracts and benefits, including healthcare program participation.
- Indiana Medicaid Exclusion List: State-level program bars capturing exclusions specific to Indiana Medicaid that may not appear in federal databases.
Healthcare facilities must conduct these database searches monthly for existing employees, not merely at hire. A single excluded employee providing services to federal program beneficiaries exposes the facility to False Claims Act liability and civil monetary penalties. Some facilities implement automated monitoring systems that alert HR departments immediately when employees appear on exclusion lists.
Disqualifying Offenses and Evaluation Criteria
ISDH regulations establish specific offense categories that permanently or temporarily bar healthcare employment, with variable lookback periods based on offense severity and patient risk correlation research. Healthcare administrators must understand these distinctions to make compliant hiring decisions. The framework balances public safety with fair chance hiring principles.
Permanently Disqualifying Convictions
Certain convictions create permanent employment bars for positions with patient access regardless of rehabilitation evidence or time elapsed since conviction. Healthcare facilities cannot employ individuals with these convictions in any patient-contact capacity without obtaining an ISDH waiver through the formal variance process.
| Offense Category | Specific Examples | Employment Restriction |
| Violent Crimes | Murder, voluntary manslaughter, aggravated assault | Permanent bar from all patient contact roles |
| Sexual Offenses | Criminal deviate conduct, sexual offenses involving minors, sexual battery | Permanent bar from all patient contact roles |
| Exploitation Crimes | Human trafficking, exploitation of endangered adults, patient abuse resulting in serious injury | Permanent bar from all patient contact roles |
Administrators discovering permanent disqualifications in existing employees must initiate immediate suspension and termination procedures to maintain facility compliance. Facilities that knowingly employ permanently disqualified individuals face enhanced penalties and potential license revocation.
Seven-Year Lookback Period Offenses
Most felony convictions trigger a seven-year disqualification period measured from conviction date, sentence completion date, or release from incarceration (whichever is latest). This category allows for rehabilitation consideration after sufficient time has elapsed. The seven-year lookback includes:
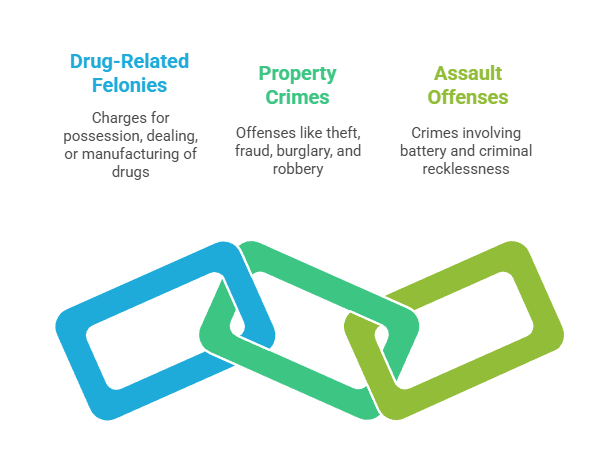
- Drug-Related Felonies: Possession, dealing, or manufacturing charges except minor possession offenses eligible for shorter lookback periods
- Property Crimes: Theft and fraud crimes valued over $750, burglary, and robbery offenses demonstrating dishonesty or violence
- Assault Offenses: Battery resulting in bodily injury, criminal recklessness involving substantial risk of serious bodily injury
Healthcare employers may consider applicants with convictions exceeding the seven-year threshold after conducting individualized assessments. Facilities should document their evaluation considering offense nature, rehabilitation evidence, references, and position-specific risk factors to demonstrate compliance with fair chance hiring principles.
Drug Offense Special Considerations
Drug-related offenses receive heightened scrutiny in healthcare settings due to controlled substance access and diversion risks. Felony dealing or trafficking convictions permanently disqualify individuals from roles with medication access. Felony possession convictions trigger a 7-year bar from such positions, while misdemeanor possession offenses may permit employment after a 3-year waiting period with documented rehabilitation.
Healthcare facilities with onsite pharmacies, medication rooms, or anesthesia supply areas must conduct enhanced screening for positions with potential controlled substance access. Some facilities implement additional safeguards such as witnessed medication waste procedures and automated dispensing system monitoring for employees with disclosed historical substance-related offenses beyond disqualification periods. These risk mitigation strategies protect both patients and the facility's DEA licensure.
Implementing Compliant Screening Procedures

Effective implementation requires standardized workflows ensuring consistent application, legal compliance, and documentation sufficiency for regulatory audits. Healthcare facilities must balance efficiency with thoroughness. The implementation process typically spans 3-4 weeks from conditional offer to start date.
Pre-Employment Process and Timing
Healthcare facilities must structure their hiring process to complete background checks after extending a conditional employment offer but before the employee's start date. The conditional offer approach complies with FCRA requirements while allowing candidates to authorize screening after demonstrating serious employer interest. Offer letters should explicitly state employment is contingent upon satisfactory background check results, drug screening completion, and credential verification.
The screening timeline requires realistic expectations to avoid compliance shortcuts. Healthcare administrators should follow this sequence:
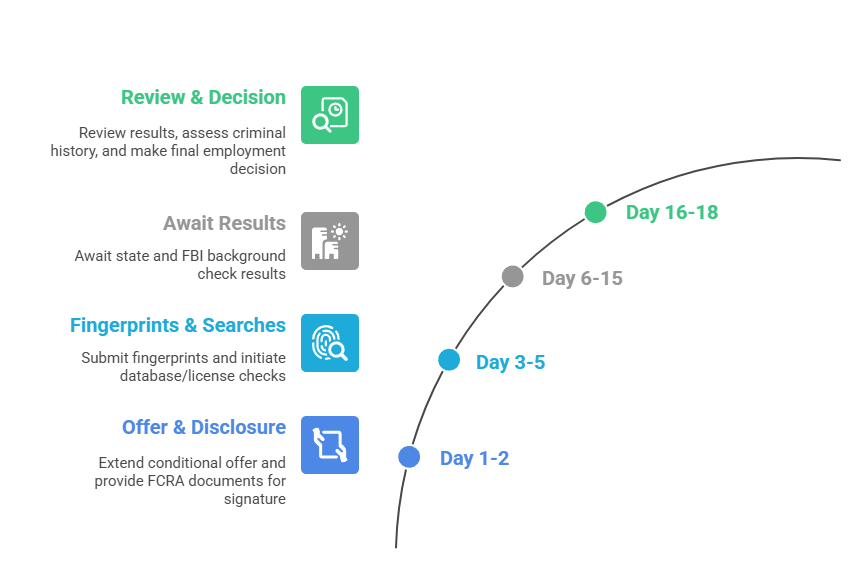
- Day 1-2: Extend conditional offer and provide FCRA disclosure documents with authorization forms for candidate signature
- Day 3-5: Submit fingerprints to approved channeling agency and initiate exclusion database searches and license verification
- Day 6-15: Await state and FBI background check results while monitoring for interim processing issues
- Day 16-18: Review results, conduct individualized assessment if criminal history identified, and make final employment decision
Facilities facing staffing emergencies may utilize expedited processing services reducing timelines to 5-7 days but should avoid pressure for incomplete screening that creates compliance gaps. Emergency staffing needs do not justify provisional employment before background check completion for patient-contact positions.
FCRA Compliance and Adverse Action
The Fair Credit Reporting Act governs employment background checks conducted through third-party screening companies. Healthcare employers must provide standalone disclosure documents explaining background check scope before obtaining written authorization. Combined disclosure-authorization forms face legal challenges and should be avoided.
When background check results may lead to adverse employment action, employers must follow specific notification procedures. Pre-adverse action requires providing candidates with a copy of the background check report and the FTC's "A Summary of Your Rights Under the Fair Credit Reporting Act." Candidates must receive reasonable time (3-5 business days recommended) to dispute inaccuracies before final adverse action.
Final adverse action requires written notice identifying the screening company, explaining the decision basis, and informing candidates of their dispute rights. Healthcare facilities should maintain documentation of all FCRA compliance steps including dates of disclosure, authorization, pre-adverse action notice, waiting period, and final adverse action notice. FCRA violations expose employers to statutory damages of $100-$1,000 per violation plus attorney's fees.
Managing Existing Employee Re-Screening
The 2025 expanded requirements mandate re-screening of current healthcare employees hired under previous standards. This creates logistical challenges for large facilities with hundreds or thousands of employees. Healthcare administrators must balance compliance deadlines with operational continuity and staff morale.
Healthcare administrators should prioritize re-screening based on patient vulnerability, access level, and compliance deadline proximity. Initial focus should target employees with unsupervised access to vulnerable populations including pediatric units, behavioral health settings, geriatric care areas, and labor/delivery departments. Secondary priority encompasses employees with controlled substance access, followed by general patient care staff and finally administrative personnel with incidental patient area access.
Facilities should communicate re-screening requirements clearly to existing staff, emphasizing that participation is a condition of continued employment. The communication strategy should include:
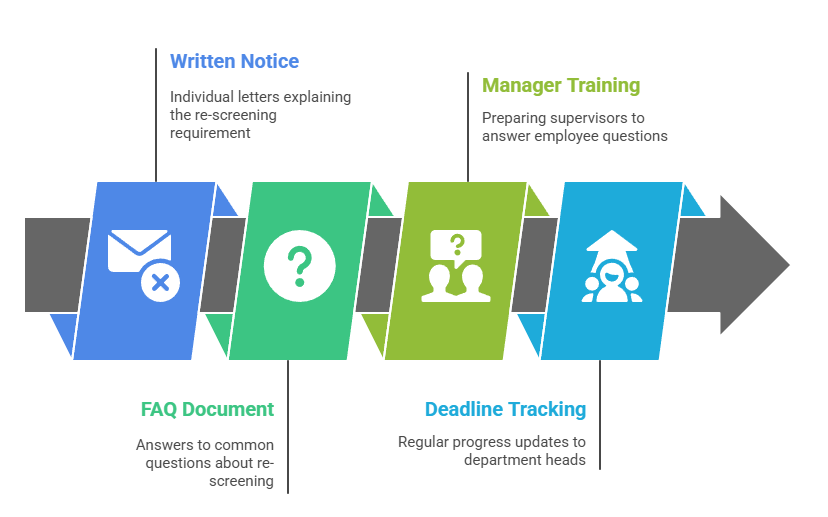
- Written Notice: Individual letters explaining the re-screening requirement, process, timeline, and employer payment of all screening costs
- FAQ Document: Answers to common questions about why re-screening is required, what happens during the process, and privacy protections
- Manager Training: Preparing supervisors to answer employee questions and address concerns about the re-screening initiative
- Deadline Tracking: Regular progress updates to department heads ensuring all employees complete fingerprinting within specified timeframes
Employers should absorb re-screening costs rather than requiring employee payment to avoid wage and hour complications and resistance that could delay compliance achievement. Most facilities budget $75-150 per existing employee for comprehensive re-screening.
Addressing Disqualifying Results in Current Staff
When re-screening reveals disqualifying offenses in current employees, healthcare facilities face complex employment decisions balancing compliance, institutional knowledge retention, and legal risks. Employees with permanent disqualifications must be removed from patient care roles immediately, with potential reassignment to non-patient-contact administrative positions if available and appropriate.
Employees with offenses within lookback periods but hired before expanded requirements present particular challenges. Some facilities have successfully negotiated ISDH variance requests for long-tenured employees with documented excellent performance and no subsequent offenses. Alternative approaches include modified duty assignments eliminating patient contact, supervisory restrictions requiring shadowing, and extended leave while pursuing expungement if legally eligible.
Penalties, Liability, and Enforcement Mechanisms
Non-compliance with Indiana healthcare background check requirements exposes facilities to multiple enforcement mechanisms and liability theories creating substantial financial and operational risks. ISDH employs progressive enforcement for background check violations. Understanding these consequences helps administrators prioritize compliance investments.
ISDH issues written warnings for first-time minor documentation gaps. More serious violations result in civil monetary penalties of $1,000 to $25,000 per violation. Violations are calculated per non-compliant employee, meaning facilities with systemic screening deficiencies face cumulative penalties potentially exceeding $500,000 for large workforce non-compliance.
Serious or repeated violations may trigger facility license suspension or revocation proceedings. This effectively terminates operations until compliance is achieved and maintained for a specified probationary period. Healthcare administrators should note that personal liability may extend to compliance officers and executives who knowingly disregard screening requirements or falsify documentation.
Federal Program Exclusion Risks
Healthcare facilities that bill Medicare or Medicaid face additional federal enforcement risks when employing excluded individuals or failing to conduct required exclusion database screening. The OIG may impose civil monetary penalties up to $10,000 per item or service provided by an excluded individual. The False Claims Act permits treble damages for knowing submissions of claims involving excluded persons.
Beyond monetary penalties, OIG may exclude the entire healthcare facility from federal program participation for employing excluded individuals. This outcome effectively terminates most hospitals' and healthcare facilities' financial viability. Corporate integrity agreements resulting from exclusion violations require expensive compliance monitoring, independent review organizations, and executive certification of compliance systems for 3-5 year periods.
Civil Liability for Patient Safety Incidents
Negligent hiring and negligent retention theories create civil liability exposure when healthcare facilities fail to conduct adequate background screening and an employee subsequently harms a patient. Plaintiff attorneys in medical malpractice and patient abuse cases routinely request employee background check documentation. Screening deficiencies dramatically strengthen liability claims and increase settlement valuations.
Juries respond particularly negatively to preventable harm cases where background check failures allowed employees with relevant criminal histories to access vulnerable patients. Verdicts in negligent hiring cases involving patient sexual assault by employees with prior sex offense convictions have exceeded $15 million. Beyond compensatory damages, some states permit punitive damages for reckless hiring practices that demonstrate conscious disregard for patient safety.
Best Practices for Healthcare Screening Programs
Leading healthcare organizations implement comprehensive screening programs exceeding minimum regulatory requirements to maximize patient safety and organizational protection. These best practices represent the standard of care emerging across the healthcare industry. Administrators should evaluate their current programs against these benchmarks.
Rather than limiting background checks to pre-employment, advanced healthcare facilities implement continuous monitoring systems. These systems alert HR to post-hire arrests, convictions, license sanctions, and exclusion database additions. Continuous monitoring particularly benefits large healthcare systems with thousands of employees where manual re-screening every few years creates substantial non-compliance risk during interim periods.
Key elements of effective continuous monitoring programs include:
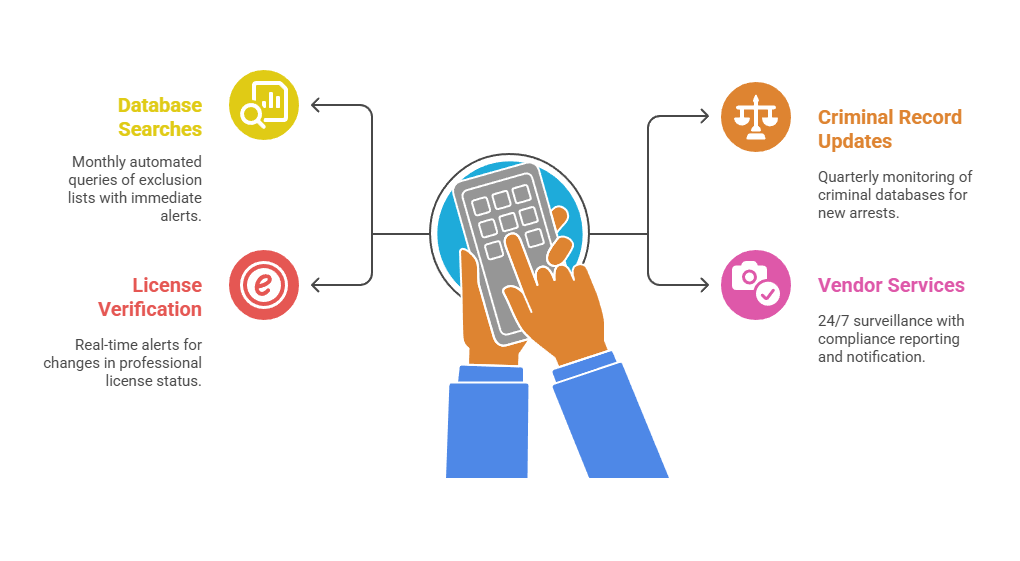
- Monthly Database Searches: Automated queries of OIG LEIE, SAM, and state Medicaid exclusion lists with immediate alerts for any employee matches
- Quarterly Criminal Record Updates: Ongoing monitoring of state and federal criminal databases for new arrests, charges, or convictions
- License Status Verification: Real-time alerts when professional licenses expire, suspend, or face disciplinary actions from state boards
- Vendor-Managed Services: Third-party monitoring providers offering 24/7 surveillance with dedicated compliance reporting and immediate notification protocols
The investment in monitoring services typically costs $5-15 per employee annually. This provides significant liability protection relative to the modest cost compared to potential damages from a preventable patient safety incident.
Vendor Management and Training
Healthcare facilities increasingly rely on contract labor, temporary agencies, locum tenens providers, and outsourced services that introduce screening compliance gaps if vendor employees aren't held to identical standards. Comprehensive vendor agreements should require contract employees meet all ISDH background check requirements before facility access. Vendor responsibility includes screening costs and documentation maintenance.
Healthcare facilities should verify vendor compliance through annual audits requesting sample employee background check documentation. Audits should review proof of exclusion database screening processes and vendor-maintained compliance attestations. Some facilities require vendors to use the healthcare organization's designated screening provider to ensure consistent standards and centralized documentation accessible during regulatory audits.
Conclusion
Indiana's expanded healthcare background check requirements represent a significant regulatory shift demanding immediate compliance attention from healthcare administrators across all facility types. The comprehensive screening framework creates substantial patient safety improvements while imposing notable implementation challenges and costs. Healthcare facilities that proactively establish compliant screening workflows, documentation systems, and continuous monitoring programs will successfully navigate the 2025 compliance deadlines while minimizing regulatory penalties. The investment in comprehensive background check infrastructure ultimately protects both vulnerable patient populations and healthcare organizations' operational viability in an increasingly scrutinized regulatory environment.
Frequently Asked Questions
What is the cost of Indiana healthcare background checks for employers?
Compliant Indiana healthcare background checks typically cost $75-150 per employee, including state criminal history ($15-25), FBI fingerprint-based search ($35-50), healthcare exclusion database screening ($10-20), and professional license verification ($15-25). Volume pricing is available for large facilities, with some screening vendors offering bundled healthcare packages reducing per-employee costs to $60-90 when screening hundreds annually. Employers typically absorb these costs rather than charging employees.
How long are Indiana healthcare background checks valid?
Indiana healthcare background checks are valid for the duration of continuous employment with the same healthcare facility. When employees transfer between healthcare organizations, new comprehensive screening is required regardless of how recently previous screening occurred. ISDH recommends re-screening existing employees every 5 years and conducting monthly exclusion database checks to identify post-hire disqualifying events throughout employment.
Can healthcare workers begin employment before background checks are completed?
No, Indiana regulations prohibit healthcare workers from providing direct patient care before background check completion and favorable results verification. Conditional offers may be extended pending screening, but employees cannot begin patient-contact duties during the processing period. Some facilities allow new employees to complete orientation and administrative tasks without patient access while awaiting results, but unsupervised patient care is strictly prohibited.
What happens if a current healthcare employee fails re-screening?
Healthcare employees who fail re-screening must be immediately removed from patient care duties pending investigation and individualized assessment. Employers should evaluate whether the disqualifying offense falls within applicable lookback periods and permits reassignment to non-patient-contact roles. Employees with permanent disqualifications must be terminated or reassigned to positions without patient access, while those with time-limited disqualifications may be eligible for leave and future reinstatement.
Are volunteer healthcare workers subject to the same background check requirements?
Yes, volunteers with potential unsupervised patient access must undergo identical background screening as paid employees, including fingerprint-based state and FBI checks, exclusion database searches, and professional license verification if providing clinical services. Healthcare facilities remain responsible for volunteer screening costs and documentation maintenance, with the same ISDH compliance requirements and potential penalties for screening failures.
Can Indiana healthcare facilities hire applicants with criminal history?
Indiana healthcare facilities may hire applicants with criminal history outside lookback periods and not involving permanently disqualifying offenses after conducting individualized assessments. Employers should evaluate the offense-job relationship, time elapsed, rehabilitation evidence, and patient safety considerations before making adverse decisions. Fair chance hiring principles encourage employment opportunities for rehabilitated individuals in positions where criminal history doesn't present unacceptable patient risk.
How do multi-state healthcare employers handle Indiana background check requirements?
Healthcare organizations operating in multiple states must comply with Indiana-specific requirements for all employees working in Indiana facilities regardless of where they were initially hired or primarily work. Employees transferring from out-of-state facilities to Indiana locations require new Indiana-compliant screening even if recently screened under another state's requirements. Multi-state employers should implement screening protocols meeting the most stringent state requirements across all locations.
What is the process for obtaining an ISDH variance for a disqualified employee?
Healthcare facilities seeking ISDH variance must submit formal requests including detailed offense description and dates, comprehensive rehabilitation evidence, character references and employment history, and proposed supervision and risk mitigation plans. ISDH evaluates variance requests case-by-case with no guaranteed approval, generally reserving variances for exceptional circumstances involving long-term rehabilitation, extraordinary extenuating circumstances, and robust ongoing monitoring proposals.
Additional Resources
- Indiana State Department of Health - Healthcare Worker Background Check Requirements
https://www.in.gov/health/phlc/oversight-and-compliance/healthcare-worker-background-checks/ - Indiana State Police - Fingerprint-Based Background Checks for Healthcare Employers
https://www.in.gov/isp/criminal-history-background-checks/ - HHS Office of Inspector General - List of Excluded Individuals and Entities (LEIE)
https://oig.hhs.gov/exclusions/ - Indiana Professional Licensing Agency - License Verification and Disciplinary Actions
https://www.in.gov/pla/licenses/ - Federal Trade Commission - Using Consumer Reports: What Employers Need to Know
https://www.ftc.gov/business-guidance/resources/using-consumer-reports-what-employers-need-know
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub

How Long Does a Background Check Take? A Complete 2025 Guide
13 Dec, 2023 • 14 min read
The Ultimate Background Check Guide
13 Dec, 2023 • 4 min read
The Ultimate Guide to Employment Background Checks
13 Dec, 2023 • 10 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.

