Alabama healthcare facilities must comply with a complex framework of federal and state-mandated background screening requirements. These requirements extend beyond basic criminal history checks to include specialized databases, professional license verification, and continuous monitoring protocols. This comprehensive guide provides healthcare HR professionals and compliance officers with the actionable regulatory framework necessary to implement compliant screening programs that protect patient safety while mitigating organizational liability risks.
Key Takeaways
- Alabama hospitals must conduct FBI fingerprint-based background checks for all direct patient care personnel as mandated by the Alabama Board of Health Administrative Code Chapter 420-5-7A-.03.
- Healthcare facilities are required to screen employees and contractors against the OIG List of Excluded Individuals/Entities (LEIE) and GSA's System for Award Management (SAM) database monthly.
- Certified Nursing Assistants (CNAs) in Alabama must complete state registry verification and abuse registry checks through the Alabama Department of Public Health before providing patient care services.
- The state's continuous monitoring requirement means healthcare employers must establish ongoing screening protocols rather than relying solely on pre-employment background checks.
- Alabama's seven-year lookback period for criminal history applies to most healthcare positions. However, certain serious offenses have no time limitation under federal exclusion guidelines.
- Medical assistant background check requirements in Alabama include both state criminal databases and the Alabama Nurse Aide Registry. This applies even though medical assistants are not licensed professionals in the state.
- Healthcare compliance background verification must be documented and retained for a minimum of five years following employee termination to satisfy Joint Commission and CMS audit requirements.
- Failure to conduct proper Alabama healthcare worker screening processes can result in civil monetary penalties up to $10,000 per violation under the Social Security Act Section 1128A.
Understanding Alabama's Regulatory Framework for Healthcare Background Screening
Alabama healthcare facilities operate under a dual regulatory structure. This structure combines state-specific requirements from the Alabama Department of Public Health with federal mandates from CMS, OIG, and other oversight agencies. The Alabama Board of Health requirements establish baseline screening standards that apply to all licensed healthcare facilities. Meanwhile, federal regulations impose additional obligations for organizations participating in government healthcare programs.
State-Level Alabama Board of Health Requirements
The Alabama Administrative Code Title 420 establishes comprehensive background screening protocols for healthcare facilities. Chapter 420-5-7A-.03 specifically requires hospitals, nursing homes, and assisted living facilities to conduct criminal background checks. These checks apply to all employees, contractors, and volunteers who have direct patient contact or access to patient records. These Alabama hospital background screening requirements mandate FBI fingerprint-based checks rather than name-based searches. This ensures a higher degree of accuracy in identity verification.
The state regulation requires facilities to screen applicants for convictions involving violent crimes, sexual offenses, theft, fraud, and controlled substance violations. Additionally, Alabama healthcare facilities must verify that applicants do not appear on the Alabama abuse registry. This registry tracks substantiated findings of patient abuse, neglect, or misappropriation of patient property. The screening process must be completed before an individual begins work. Limited exceptions exist for conditional employment pending final clearance results.
Federal Requirements for Medicare and Medicaid Participation
Healthcare organizations accepting Medicare or Medicaid reimbursement must comply with federal screening requirements that often exceed state minimums. The Affordable Care Act Section 6401 established enhanced screening protocols. These protocols require monthly searches of the OIG LEIE and SAM databases. These exclusion lists identify individuals and entities prohibited from participating in federal healthcare programs. Prohibitions stem from fraud, abuse, or license revocations.
CMS requires healthcare facilities to implement screening protocols that verify professional licenses, board certifications, and controlled substance registrations for all clinical staff. The healthcare compliance background verification process must include primary source verification. This means employers cannot rely solely on copies of licenses or credentials provided by applicants. Facilities must also conduct education verification for positions requiring specific degrees or certifications. They must confirm graduation directly with accredited institutions.
Joint Commission and Accreditation Body Standards
Healthcare facilities seeking Joint Commission accreditation must satisfy additional screening requirements outlined in the Human Resources Management Standards. Standard HR.01.06.01 requires organizations to conduct background checks appropriate to staff positions and consistent with federal and state law. The Joint Commission emphasizes competency verification. Facilities must implement primary source verification for licenses, education, and training credentials.
Accreditation standards also mandate that facilities establish policies defining disqualifying offenses and the evaluation process for applicants with criminal histories. These policies must demonstrate consistency with applicable laws. They must also provide a framework for individualized assessment when required by EEOC guidance. Consequently, healthcare organizations must document their screening criteria. They must maintain comprehensive personnel files that evidence compliance with all applicable requirements.
Essential Components of CNA Background Screening in Alabama
Certified Nursing Assistants represent the largest category of direct care workers in Alabama healthcare facilities. Therefore, CNA background screening Alabama protocols are particularly critical to organizational compliance. The state maintains specific requirements for CNA screening that differ from general healthcare worker protocols. These differences exist due to the vulnerable populations these professionals serve and their registry-based certification system.
Alabama Nurse Aide Registry Verification
Before a CNA can be employed in Alabama, facilities must verify current registration through the Alabama Nurse Aide Registry. The Alabama Department of Public Health maintains this registry. This verification process confirms several critical elements about the individual's qualifications and history:

- Training completion: Confirms the individual completed an approved training program
- Competency examination: Verifies passage of the state competency examination
- Registration status: Ensures maintenance of active, unencumbered registration
- Abuse findings: Indicates any substantiated findings of abuse, neglect, or misappropriation that would prohibit employment
Alabama regulations require facilities to complete registry verification within 20 days of hire if hiring a CNA from another state. During this period, the facility may employ the individual while awaiting reciprocity processing. However, they must maintain documentation of the verification request.
Criminal Background Check Requirements for CNAs
Beyond registry verification, Alabama hospital background screening requirements mandate comprehensive criminal history checks for all CNAs. These checks must include fingerprint-based FBI searches. The searches identify both in-state and out-of-state convictions. The Alabama Department of Public Health provides approved vendors for fingerprinting services. Facilities must use these designated providers to ensure compliance with state protocols.
The screening must identify convictions for offenses defined as disqualifying under Alabama Code § 38-13-3. This includes crimes involving violence, sexual offenses, financial exploitation, and controlled substance violations. However, Alabama law requires individualized assessment for certain offenses more than five years old. This balances public safety concerns with fair chance employment principles.
Implementing Compliant Background Screening Processes

Establishing a compliant screening program requires healthcare facilities to develop systematic processes. These processes must address timing, vendor selection, record retention, and ongoing monitoring. The Alabama healthcare worker screening process must be consistently applied across all positions. At the same time, it must maintain flexibility to address role-specific risk factors. Facilities that implement structured protocols reduce compliance risks. They also create defensible documentation during regulatory surveys.
Pre-Employment Screening Timeline and Procedures
Alabama regulations permit conditional offers of employment pending background check completion. However, they prohibit unsupervised patient contact before clearance. Most healthcare facilities implement a structured timeline that includes initiating background checks within 24 hours of a conditional offer. Results are typically available within 5-7 business days for in-state checks. FBI fingerprint results require 7-14 business days. However, processing times can vary seasonally.
Healthcare compliance background verification protocols should include verification of professional licenses immediately upon receipt of an application for clinical positions. Most state licensing boards provide online verification systems. These systems allow instant confirmation of license status, expiration dates, and disciplinary actions. Facilities should document the verification date and source. They should maintain screenshots or printed confirmation pages in personnel files.
Vendor Selection and FCRA Compliance
Healthcare organizations using third-party background screening vendors must ensure these providers comply with the Fair Credit Reporting Act (FCRA). The FCRA governs consumer reporting agencies. It establishes specific disclosure, authorization, and adverse action requirements that healthcare employers must follow. Understanding these requirements protects facilities from costly litigation. It also ensures applicants receive fair treatment throughout the screening process.
Critical FCRA compliance elements for healthcare background screening include:
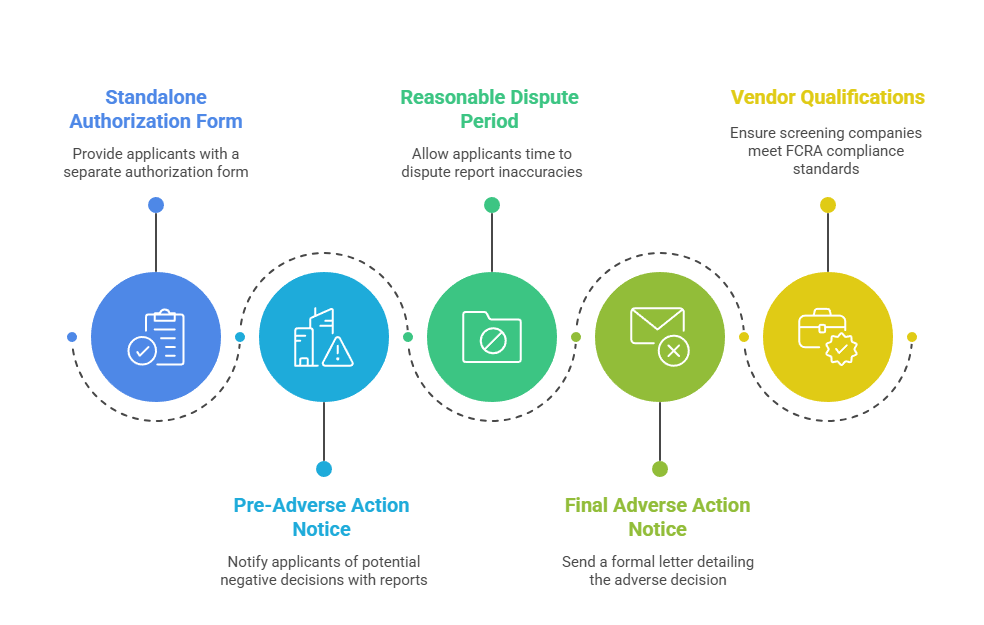
- Standalone authorization: Facilities must provide applicants with clear, standalone authorization forms separate from employment applications before initiating background checks
- Pre-adverse action notice: Employers must provide applicants with copies of background reports and FCRA rights summaries before making negative employment decisions
- Reasonable dispute period: Applicants must receive at least 5 business days to dispute report inaccuracies before final adverse action
- Final adverse action notice: Employers must send formal adverse action letters including screening company contact information and dispute rights
- Vendor qualifications: Background screening companies must demonstrate compliance with FCRA requirements and maintain appropriate accreditations
Healthcare facilities should select vendors with experience in healthcare compliance background verification. This ensures reports include all required database searches. It also ensures appropriate formatting for regulatory audits. Experienced vendors understand the unique requirements of Alabama hospital background screening. They can guide facilities through complex compliance scenarios.
Continuous Monitoring and Periodic Re-Screening
Alabama Board of Health mandates that facilities implement systems to identify arrests, convictions, license actions, and exclusion list additions affecting current employees. The continuous monitoring obligation extends Alabama hospital background screening requirements beyond the initial hire date. This creates ongoing compliance responsibilities. Many facilities initially overlook these responsibilities when developing their screening programs.
Most healthcare organizations satisfy this requirement through monthly exclusion list screening. They also use automated license verification systems that alert HR departments to status changes. Some facilities implement annual or biennial criminal background re-screening for high-risk positions. These positions involve controlled substance access or vulnerable populations. While not explicitly required by Alabama regulation, periodic re-screening represents a best practice. It protects facilities from negligent retention liability.
Position-Specific Screening Requirements in Alabama Healthcare
Different healthcare roles carry varying levels of patient interaction, access to controlled substances, and regulatory oversight. Accordingly, Alabama healthcare facilities should implement tiered screening programs. These programs apply enhanced checks to higher-risk positions while maintaining baseline requirements for all personnel. This risk-based approach satisfies regulatory requirements. It also efficiently allocates compliance resources.
Licensed Clinical Staff Screening Protocols
Physicians, registered nurses, pharmacists, and other licensed professionals require comprehensive screening. This screening includes primary source license verification, board certification confirmation, and DEA registration validation where applicable. The Alabama Board of Health requirements mandate that facilities verify licenses at hire. They must also implement systems to monitor expiration dates and disciplinary actions throughout employment. For physicians, facilities must also complete National Practitioner Data Bank (NPDB) queries. Medical staff bylaws and credentialing protocols require these queries.
Though the NPDB is not technically a background check database, it serves a similar function. It identifies malpractice payments, adverse clinical privilege actions, and professional society membership sanctions. NPDB queries must be repeated every two years for physicians with active privileges. This creates ongoing verification obligations beyond initial credentialing. Facilities must systematically track these obligations to maintain compliance.
Medical Assistant and Unlicensed Personnel Requirements
Medical assistants occupy a unique position in Alabama healthcare facilities. The state does not license or certify this profession. Despite the lack of licensure, medical assistant background check requirements mirror those for CNAs. This is due to their direct patient care responsibilities. They also maintain access to protected health information. This creates significant privacy and security obligations.
Facilities should conduct the same FBI fingerprint checks, abuse registry searches, and exclusion list verifications used for certified positions. Unlicensed assistive personnel, including patient care technicians, unit secretaries, and environmental services staff, require background screening appropriate to their access levels. Alabama healthcare worker screening processes should document the risk assessment used to determine screening depth for each position category. This demonstrates thoughtful application of regulatory requirements.
Contract, Temporary, and Agency Personnel
Healthcare facilities maintaining relationships with staffing agencies and contract service providers must ensure these vendors conduct background screening equivalent to facility standards. The Alabama hospital background screening requirements apply regardless of employment structure. This means contracted CNAs must meet the same registry and criminal background standards as facility-employed CNAs. This creates verification challenges for HR departments.
Best practice involves requiring vendors to provide evidence of background screening completion for each individual before granting facility access. This documentation should include verification dates, databases searched, and clearance confirmation. Some healthcare organizations require staffing agencies to use the facility's designated screening vendor. This ensures consistency and facilitates audit documentation.
Evaluating Criminal History and Disqualifying Offenses
Alabama law and federal regulations establish certain automatic disqualifications. They also require individualized assessment for other criminal convictions. Healthcare HR professionals must understand these distinctions to make legally compliant employment decisions. Balancing patient safety with fair chance employment principles requires structured evaluation processes and comprehensive documentation.
Mandatory Exclusions Under Federal and State Law
Federal law prohibits healthcare facilities from employing individuals excluded from Medicare and Medicaid participation. These exclusions result from convictions related to healthcare fraud, patient abuse, or controlled substance offenses. The Social Security Act Section 1128 establishes mandatory exclusion periods. It also creates substantial financial penalties for non-compliance:
| Exclusion Type | Duration | Violation Penalty |
| Program-Related Crimes | Minimum 5 years | $10,000 per service provided |
| Patient Abuse | Permanent | $10,000 per service provided |
| Controlled Substance Convictions | Minimum 5 years | $10,000 per service provided |
Alabama Code § 38-13-3 identifies state-level disqualifying offenses for healthcare facility employment. These include violent felonies, sexual offenses, exploitation of vulnerable adults, and controlled substance trafficking. These disqualifications apply permanently for certain serious offenses. However, the statute allows facilities to request waivers from the Alabama Department of Public Health. Waivers may be granted for convictions older than five years if the individual demonstrates rehabilitation.
EEOC Guidance and Individualized Assessment
For offenses not subject to mandatory exclusion, the Equal Employment Opportunity Commission requires employers to conduct individualized assessments. Employers cannot implement blanket conviction-based exclusion policies. EEOC Enforcement Guidance from 2012 establishes a three-factor analysis. Healthcare facilities must apply this analysis when evaluating criminal history. The analysis examines the nature and gravity of the offense, time elapsed since the conviction, and the nature of the job sought.
Alabama healthcare facilities should implement structured assessment protocols. These protocols must document consideration of these factors for each applicant with reportable criminal history. The assessment should consider evidence of rehabilitation. This includes educational achievements, employment history, and character references obtained since the conviction. Facilities should maintain written policies defining their assessment process. They should train hiring managers on consistent application. This minimizes disparate impact discrimination risks while protecting patient safety.
Background Check Lookback Periods and Reporting Limitations
Alabama law establishes a seven-year lookback period for most criminal background checks. This means convictions older than seven years need not be reported by screening vendors. However, healthcare positions often qualify for exceptions to this limitation. They involve working with vulnerable populations or access to controlled substances.
The Fair Credit Reporting Act allows expanded reporting for positions with annual salaries exceeding $75,000. However, this threshold sees limited application for many healthcare roles. Federal exclusion requirements have no time limitation. An individual excluded for a healthcare fraud conviction 15 years ago remains excluded absent formal reinstatement by OIG. This creates a practical requirement for healthcare facilities to search exclusion databases. The search must occur regardless of how long ago the underlying offense occurred.
Documentation, Record Retention, and Audit Preparation
Comprehensive documentation of background screening activities protects healthcare facilities during regulatory surveys, accreditation reviews, and employment-related litigation. Alabama healthcare facilities must maintain screening records in compliance with both federal retention requirements and state personnel file regulations. Systematic documentation practices transform compliance from a reactive burden into a strategic asset. They demonstrate organizational commitment to patient safety.
Required Documentation and Personnel File Contents
Each employee's personnel file should contain comprehensive documentation of all completed background screening components. Alabama Board of Health surveyors routinely audit personnel files during licensing inspections. They select random samples to verify background check completion. Essential documentation elements include:
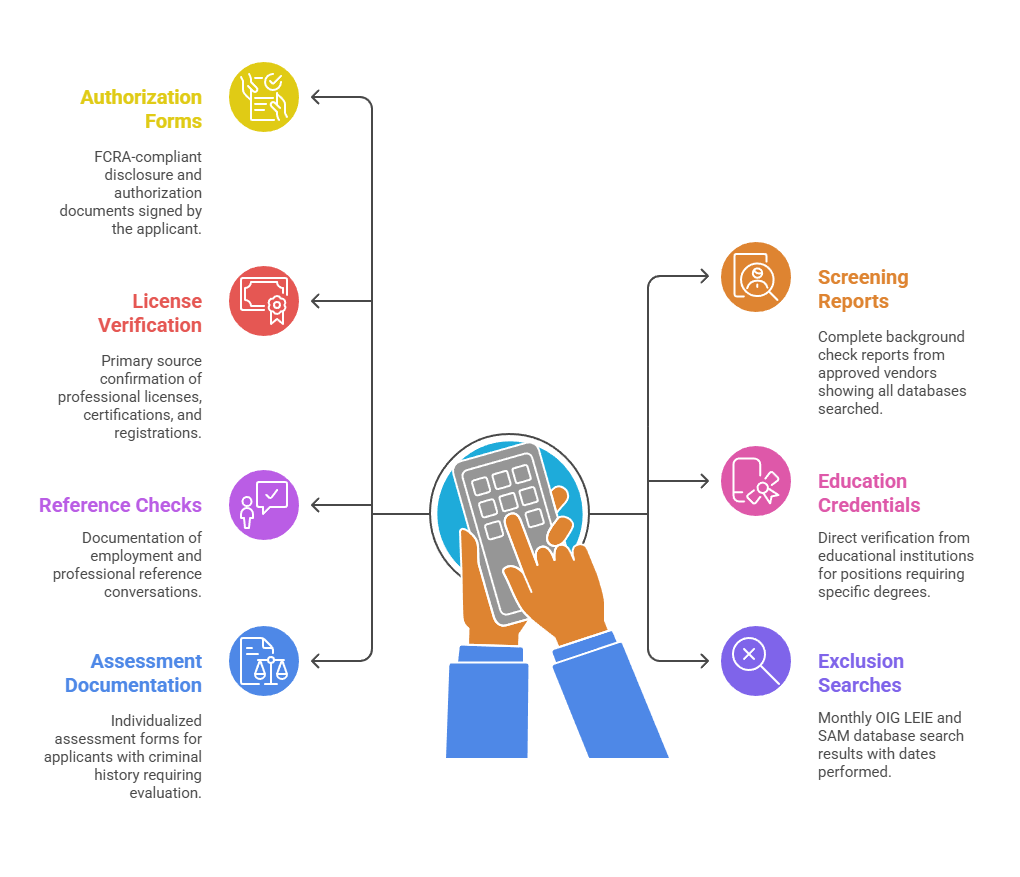
- Authorization forms: FCRA-compliant disclosure and authorization documents signed by the applicant
- Screening reports: Complete background check reports from approved vendors showing all databases searched
- License verification: Primary source confirmation of professional licenses, certifications, and registrations
- Education credentials: Direct verification from educational institutions for positions requiring specific degrees
- Reference checks: Documentation of employment and professional reference conversations
- Exclusion searches: Monthly OIG LEIE and SAM database search results with dates performed
- Assessment documentation: Individualized assessment forms for applicants with criminal history requiring evaluation
Facilities should implement internal audit protocols that periodically review personnel files for completeness before external surveys occur. Documentation should clearly indicate the date each screening component was completed. It should also show the source of information and the individual who performed the verification.
Retention Requirements and Electronic Record Systems
Federal regulations require healthcare facilities to retain personnel records, including background screening documentation, for a minimum of five years following employee termination. Some state regulations and accreditation standards impose longer retention periods. Therefore, seven-year retention has become a common best practice among Alabama healthcare organizations.
Electronic document management systems facilitate this retention while improving accessibility during audits. Healthcare facilities implementing electronic personnel file systems must ensure appropriate security controls. These controls protect confidential background information. The Fair Credit Reporting Act requires that employers maintain reasonable procedures. These procedures protect the confidentiality of consumer reports. They also ensure proper disposal of these documents when no longer needed.
Common Compliance Challenges and Risk Mitigation Strategies
Healthcare facilities implementing Alabama hospital background screening requirements encounter predictable challenges. These challenges can compromise compliance without proper planning. Understanding these common pitfalls enables HR professionals to design systems that prevent rather than remedy compliance gaps. Proactive risk management protects patient safety. It also reduces the likelihood of costly regulatory violations.
Timing Issues and Conditional Employment Practices
One frequent compliance violation involves allowing employees to begin work before background check completion. Alabama regulations permit conditional employment but prohibit unsupervised patient contact before clearance. Some facilities misinterpret this provision. They allow conditional employees to work clinical units with minimal supervision. This creates both regulatory violations and patient safety risks. These risks can result in serious consequences during state surveys.
Best practice involves restricting conditional employees to orientation activities, competency training, and administrative tasks until full clearance is documented. Facilities should implement electronic tracking systems. These systems prevent badge activation or EHR access until all screening components are verified complete. HR departments should establish escalation protocols for background checks exceeding expected turnaround times. This ensures hiring managers understand restrictions on conditional employees. It also prevents premature clinical assignments.
Multi-State Workforce Considerations
Healthcare facilities located near state borders or employing traveling clinicians must navigate multi-jurisdictional background screening requirements. An employee who holds licenses in Alabama and neighboring states may have disciplinary actions in one jurisdiction not reflected in others. Similarly, criminal convictions in border states may not appear in Alabama-specific database searches. This creates significant gaps in screening comprehensiveness.
Comprehensive healthcare compliance background verification for multi-state workers should include license verification in all states where the individual holds or previously held credentials. Criminal background checks should cover states of current residence and previous residence within the past seven years. Facilities using traveling nurses or contract therapists should require vendors to provide multi-state screening documentation before granting facility access.
Monitoring Screening Vendor Compliance
Healthcare facilities remain ultimately responsible for background screening accuracy even when using third-party vendors. However, many organizations fail to audit vendor performance. They also fail to verify that reports include all required database searches. Implementing systematic vendor oversight protects facilities from compliance gaps. These gaps emerge during regulatory surveys when screening deficiencies are discovered.
Effective vendor audit programs should include these quarterly review components:
- Report completeness review: Sample background reports to verify inclusion of all required databases per facility policy and regulatory mandates
- Turnaround time analysis: Track vendor compliance with service level agreements for screening completion timelines
- FCRA compliance verification: Confirm adverse action procedures follow Fair Credit Reporting Act requirements with proper notice and waiting periods
- Database search accuracy: Validate that searches include appropriate jurisdictions based on applicant address history
- Account representative accessibility: Ensure direct contact with vendor representatives who understand healthcare-specific screening requirements rather than general customer service departments
HR departments should maintain direct relationships with vendor account representatives who understand healthcare-specific screening requirements. Regular vendor performance reviews create accountability. They also ensure facilities receive the quality service necessary for regulatory compliance and patient safety.
Conclusion
Compliant implementation of Alabama hospital background screening requirements demands systematic processes. These processes must integrate state regulatory mandates, federal exclusion protocols, and accreditation standards into cohesive screening programs. Healthcare HR professionals must balance patient safety imperatives with fair chance employment principles. They must apply individualized assessment to criminal history while maintaining zero tolerance for mandatory exclusions. Success requires selecting experienced screening vendors, documenting all verification activities comprehensively, and implementing continuous monitoring systems. By approaching background screening as an ongoing compliance function rather than a one-time hiring task, Alabama healthcare facilities protect patients, satisfy regulatory obligations, and minimize organizational liability exposure.
Frequently Asked Questions
What criminal convictions permanently disqualify someone from healthcare employment in Alabama?
Alabama Code § 38-13-3 establishes permanent disqualifications for convictions involving violent felonies against vulnerable adults. It also covers sexual offenses including rape and sexual abuse. Additionally, exploitation or abuse of adults in healthcare facilities results in permanent disqualification. Federal law adds permanent exclusions for healthcare fraud convictions and patient abuse in any setting receiving Medicare or Medicaid funding.
How often must Alabama hospitals check employees against the OIG exclusion list?
The Centers for Medicare & Medicaid Services requires monthly screening of all employees, contractors, and vendors. Facilities must search the OIG List of Excluded Individuals/Entities (LEIE) and the General Services Administration's System for Award Management (SAM) exclusion database. This monthly frequency ensures facilities identify exclusions promptly. Most healthcare organizations implement automated monthly screening systems that flag newly excluded individuals for immediate action.
Are medical assistants in Alabama subject to the same background check requirements as CNAs?
Although Alabama does not license or certify medical assistants, healthcare facilities typically apply the same background screening requirements used for CNAs. Both positions involve direct patient care and access to protected health information. Medical assistant background check requirements should include FBI fingerprint-based criminal history searches, Alabama abuse registry verification, and monthly OIG exclusion list screening.
What is the difference between name-based and fingerprint-based background checks?
Name-based background checks search criminal databases using identifying information such as name, date of birth, and Social Security number. Fingerprint-based checks use biometric identification to ensure accurate matching. Alabama Board of Health requirements mandate fingerprint-based FBI checks for healthcare workers. They eliminate false positives from name similarities and identify out-of-state convictions that might be missed in name-based searches.
Can Alabama healthcare facilities hire someone with a criminal record?
Yes, but the decision depends on offense type, time elapsed, position applied for, and evidence of rehabilitation. Federal and Alabama law establish certain mandatory exclusions for serious offenses. However, most convictions require individualized assessment per EEOC guidance. Healthcare facilities should implement structured evaluation processes. These processes examine offense nature and gravity, relevance to job duties, and rehabilitation evidence.
How long does the Alabama CNA background check process typically take?
Most Alabama CNA background screening processes require 7-14 business days for completion. However, timing varies based on fingerprinting appointment availability and FBI processing volume. The Alabama Nurse Aide Registry verification typically returns results within 1-2 business days for in-state searches. Reciprocity verification from other states may require 10-20 business days.
What happens if an Alabama healthcare worker is excluded after being hired?
When a current employee is added to the OIG exclusion list or SAM database, the healthcare facility must immediately remove the individual from duties generating Medicare or Medicaid claims. Federal law requires termination or reassignment to positions not funded by federal healthcare programs. The facility faces civil monetary penalties up to $10,000 per excluded person service if it fails to identify and remove the individual promptly.
Are volunteers and students subject to the same background check requirements as employees?
Yes, Alabama hospital background screening requirements apply to volunteers, students, and any other individuals with direct patient contact or access to patient information. Compensation status does not matter. The Alabama Board of Health Administrative Code explicitly includes volunteers in background check mandates. Patient safety risks exist regardless of employment status.
Additional Resources
- Alabama Department of Public Health - Nurse Aide Registry Information
https://www.alabamapublichealth.gov/nurse-aide-registry/ - HHS Office of Inspector General - List of Excluded Individuals/Entities (LEIE)
https://oig.hhs.gov/exclusions/ - Alabama Board of Health Administrative Code - Healthcare Facility Regulations
https://www.alabamapublichealth.gov/rules/ - EEOC Enforcement Guidance on Criminal Background Checks
https://www.eeoc.gov/laws/guidance/arrest-conviction-records - Federal Trade Commission - Fair Credit Reporting Act Compliance Resources
https://www.ftc.gov/legal-library/browse/statutes/fair-credit-reporting-act - Centers for Medicare & Medicaid Services - Provider Enrollment and Background Screening
https://www.cms.gov/medicare/enrollment-renewal/providers-suppliers - Joint Commission - Human Resources Management Standards
https://www.jointcommission.org/standards/standard-faqs/hospital-and-hospital-clinics/ - National Practitioner Data Bank - Healthcare Integrity and Protection Data Bank
https://www.npdb.hrsa.gov/
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub

How Long Does a Background Check Take? A Complete 2025 Guide
13 Dec, 2023 • 14 min read
The Ultimate Background Check Guide
13 Dec, 2023 • 4 min read
The Ultimate Guide to Employment Background Checks
13 Dec, 2023 • 10 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.

