In the healthcare industry, the safety and well-being of patients are paramount. To ensure a safe environment, hospitals must implement stringent measures when hiring new staff. One critical component is conducting background checks on potential employees. But are background checks required by law for hospitals? This comprehensive guide will explore healthcare background check requirements, hospital employment screening laws, and the legal nuances that hospitals must navigate to maintain compliance.
Key Takeaways
- Conducting background checks in healthcare is crucial for safeguarding patient safety and maintaining trust within hospitals.
- Utilizing comprehensive checks that include criminal history, employment verification, and education confirmation minimizes the risk of hiring individuals with past misconduct.
- Adhering to the Fair Credit Reporting Act ensures transparency and fairness in the hiring process, requiring clear candidate consent before conducting any background checks.
- Consistent application of OIG Exclusion Checks helps hospitals avoid the risks associated with hiring individuals excluded from federal healthcare programs.
- Implementing standardized hiring procedures that adapt to legal updates strengthens hospital operations and supports a trustworthy work environment.
Introduction
Ensuring patient safety and trust is non-negotiable in healthcare settings. Hospitals are expected to maintain a safe environment where patients and their information are protected. A critical part of this responsibility falls on the hiring process. Background checks serve as a cornerstone for assessing the suitability of potential staff members. They help verify that those who interact with vulnerable populations have the integrity and qualifications needed for such trust-intensive roles. This guide will walk you through the complexities of hospital background checks, from understanding what the law mandates to adopting best practices. Whether you're involved in hiring or seeking a position in healthcare, being informed is key to navigating these protocols effectively.
Understanding Healthcare Background Check Requirements
Background checks in healthcare are not just a procedural formality; they are a necessity. Hospitals have a fundamental duty to ensure the safety and trust of their patients. Without rigorous checks, the risk of hiring individuals with past misconduct or fraudulent credentials increases, undermining the trust crucial to patient care.
A comprehensive background check typically includes several key components. First is a criminal history check, which identifies any past criminal convictions that may pose a risk to patients or the hospital. Then, employment verification ensures that the candidate’s job history aligns with what they have claimed, confirming both qualifications and experience. Education confirmation ensures that applicants have the necessary academic credentials for their roles.

Another critical aspect is the OIG exclusion check. The Office of Inspector General keeps a list of individuals and entities excluded from participating in federally funded healthcare programs. Hiring someone on this list can lead to severe consequences, including the loss of federal funding. This makes the OIG check indispensable.
The Fair Credit Reporting Act (FCRA) also plays a significant role in healthcare background checks. The FCRA mandates that checks are conducted fairly and transparently. It requires employers to inform candidates that a background check will be conducted and to obtain their consent. If the background check results in a decision not to hire, the applicant must be notified and given a chance to respond.
In the end, thorough background checks are a legal and ethical obligation. They not only protect patients but also help maintain a reliable and professional workforce. Are you doing enough to ensure your hospital’s hiring practices meet these critical standards?
Hospital Employment Screening Laws
Navigating employment screening laws in hospitals requires clear understanding of both state and federal regulations. While federal laws set a baseline through legislation like the Fair Credit Reporting Act (FCRA), state laws can introduce additional layers. Some states might impose stricter rules, for example, mandating specific checks or licensing board verifications that aren't covered federally.
It's crucial to know the federal laws that apply. The FCRA is central, requiring clear disclosure and candidate consent before performing checks. If an adverse decision results from a check, hospitals must follow FCRA protocols, like sending pre-adverse action notifications and the candidate's right to dispute findings.
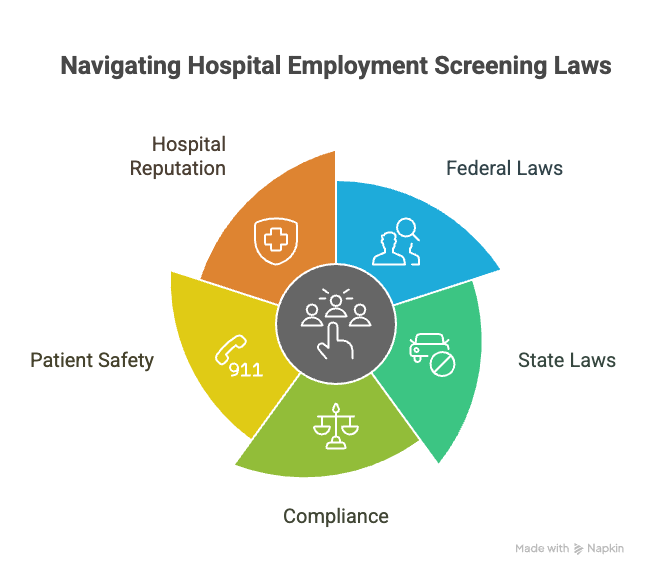
State-specific requirements vary. California, for instance, has restrictions on what criminal history can be considered, while Texas requires specific healthcare-related checks. Understanding these differences helps ensure compliance and avoid legal pitfalls.
Failing to comply with these laws can have serious repercussions, including fines and legal action. It puts patient safety and the hospital's reputation at risk. To stay compliant, regularly review and update policies based on legal changes and ensure all hiring managers understand the requirements.
Consideration of employment laws is not just about ticking boxes. It's about maintaining a safe environment for patients and staff alike. Make sure your practices not only meet legal standards but also support your mission of providing quality care.
The Importance of Background Checks in Healthcare
Conducting background checks in healthcare isn't just about ticking boxes. It's about accountability and prevention. The stakes are high; one oversight can lead to malpractice or put patients at risk. By screening thoroughly, hospitals can ensure that individuals with histories of misconduct or incompetence don't get a foothold in environments where trust and safety are non-negotiable.
The healthcare sector handles sensitive data daily. Patients trust hospitals with their personal, often intimate, information. It's crucial that the people with access to this data are vetted meticulously. Background checks help institutions verify that potential hires respect and protect patient confidentiality. Without such checks, breaches in data security could become more common, damaging reputations and leading to costly legal consequences.
Beyond security and safety, background checks foster an environment of trust and collaboration among healthcare professionals. When team members know that each has been vetted for competency and character, it builds confidence and respect within the group. When you hire, you're not just adding to payroll; you're building a team that patients will trust with their lives. So, asking yourself: who am I bringing on board, and can they be trusted with our mission? This reflection is integral to every hire.
OIG Exclusion Check: A Deeper Dive
An OIG Exclusion Check is a specific background screening that identifies individuals and entities excluded from participating in federal healthcare programs. The Office of Inspector General (OIG) maintains a list of these individuals and organizations, known for violations such as fraud or patient abuse.
When a hospital hires someone on this exclusion list, it risks more than just a bad hire. It faces potential civil monetary penalties and could also lose federal funding—an outcome that can financially harm any healthcare provider. Integrating OIG checks into hiring practices is not just wise; it’s essential for compliance and risk mitigation.
To perform OIG checks effectively, your hospital should establish a routine screening process. Before employment, run the checks and repeat them regularly throughout employment. Make it a part of your standard hiring workflow to ensure that no red flags slip through the cracks. By consistently applying these checks, you safeguard your institution from legal and financial liabilities. Are these checks part of your current hiring process? They should be.
FCRA and Legal Compliance in Hospital Hiring
The Fair Credit Reporting Act (FCRA) plays a vital role in hospital hiring practices. It is designed to ensure fairness and accuracy in background checks, requiring transparency and consent from job candidates. When a hospital conducts a background check, the FCRA mandates that candidates must provide written consent before any checks are performed. This means you must have candidates sign a clear and conspicuous disclosure, stating that a report may be used for employment decisions.
If a background check reveals issues that might lead to a decision not to hire, the FCRA has specific guidelines on handling adverse actions. First, you must provide the candidate with a "pre-adverse action" notice, including a copy of the report and a summary of their rights under the FCRA. This gives them the chance to dispute any inaccuracies. Should you choose to proceed with not hiring, you then send a "post-adverse action" notice, detailing the decision and providing information for the candidate to obtain a copy of the report.
Compliance with the FCRA isn't merely about avoiding legal trouble—it's about creating a fair process for candidates. Keeping candidates informed and ensuring accuracy in reports fosters trust and builds a reputable hiring environment. Have you reviewed your hospital’s FCRA compliance processes recently?
Best Practices for Hospital Background Checks
Create standardized procedures for conducting background checks within your hospital. A clear, consistent approach across all departments minimizes confusion and ensures everyone follows the same rules.
Keep policies updated. Laws change, and so should your practices. Schedule regular reviews to stay compliant. Train staff on these updates to keep everyone informed and capable of proper implementation.
Balance thoroughness with fairness. While it's crucial to conduct comprehensive checks, ensure you respect candidates' rights. Provide clear explanations of the process and follow legal protocols for disclosures and consent.
Use a mix of methods tailored to different roles. Customize the depth and nature of the background check to fit the job type. For example, positions with patient contact may require more extensive checks than administrative roles.
Document everything. Keep records of all screenings conducted and decisions made. Documentation offers protection in case your process is ever questioned legally.
Establish a review process for adverse findings. If a check reveals potential issues, have a structured system for evaluating their relevance to the job. Fair assessments help maintain integrity in your hiring process.
Conclusion
Background checks are essential in healthcare to ensure patient safety and maintain trust. Hospitals must navigate a complex legal landscape, balancing compliance and thorough screening. Both federal and state laws guide hospitals in conducting these checks, with laws like the Fair Credit Reporting Act playing a crucial role. Non-compliance with these laws can lead to significant legal repercussions, underscoring the importance of adhering to established guidelines.
Healthcare facilities benefit from standardized procedures that maintain uniformity across the organization. Regular updates and training for staff help in keeping their practices aligned with legal changes, maintaining a balance between thoroughness and fairness. By venturing into this disciplined approach, hospitals not only protect their patients but also cultivate a trustworthy and effective work environment. Staying informed and vigilant remains crucial in this ever-evolving field.
Resources
Finding reliable resources can enhance your understanding of background check requirements in the healthcare sector. Here's a collection of helpful links:
- Most Common Background Check Questions: This resource covers frequently asked questions that you might encounter during the background check process.
- Professional Background Screening Association (PBSA): The PBSA offers valuable insights and updates on industry standards for background checks. As a reputable organization, their resources can guide both employers and individuals on best practices and compliance.
These links are designed to support your grasp of the complexities involved in healthcare background checks. Dive into these resources to stay informed and ensure your processes align with legal expectations.
Frequently Asked Questions (FAQs)
Are hospitals legally required to do background checks on employees?
Hospitals are not universally mandated by federal law to conduct background checks on employees. However, many states and accrediting bodies require them. Background checks help ensure patient safety and mitigate risks.
What types of background checks do hospitals conduct?
Hospitals typically conduct criminal background checks, verification of education and professional licenses, and checks for any history of abuse or malpractice. They might also perform drug screening and reference checks.
Do hospitals check the OIG exclusion list?
Yes, hospitals routinely check the Office of Inspector General (OIG) exclusion list to ensure they do not hire individuals or entities excluded from participation in federal healthcare programs.
Are volunteers and contractors in hospitals background checked?
Yes, hospitals often perform background checks on volunteers and contractors to ensure patient safety and maintain compliance with regulations. The level of scrutiny may vary depending on the individual's role and access to patients.
What happens if a hospital hires someone on the exclusion list?
Hiring someone on the exclusion list can result in severe penalties for hospitals, including fines and exclusion from federal healthcare programs. It can damage a hospital’s reputation and financial standing.
How often do hospitals update their background checks?
Hospitals may periodically update background checks, particularly for employees in sensitive roles. This frequency can depend on hospital policy and state regulations.
Do hospitals verify previous employment during background checks?
Yes, verifying past employment is a common part of a hospital’s background check process. This helps confirm experience and credibility.
Are background checks the same for all hospital workers?
No, the level of scrutiny can differ based on the role. Clinical staff may undergo more comprehensive checks compared to administrative staff due to their direct interaction with patients.
Can an employee dispute findings in a background check?
Yes, employees have the right to dispute any incorrect information found in their background check. Hospitals should provide them with a copy of the report for this purpose.
Definitions
Background Check
A background check is a process employers use to review a candidate's history. It often includes criminal records, employment history, education verification, and references. In healthcare, this step helps confirm that job applicants can be trusted to work with patients and handle sensitive information.
Employment Verification
Employment verification confirms the accuracy of a candidate’s past job titles, dates of employment, and sometimes performance. It's a way for healthcare employers to validate that candidates have the experience they claim. Mistakes or lies in work history can indicate reliability concerns.
OIG Exclusion Check
An OIG Exclusion Check screens candidates against the Office of Inspector General’s list of individuals barred from participating in federal healthcare programs. People land on this list for reasons like fraud or patient abuse. Hiring someone on it risks penalties and federal funding loss.
Fair Credit Reporting Act (FCRA)
The FCRA is a federal law that sets rules for how employers use background checks in hiring. It requires written consent from the candidate before checks are done. If something negative appears, employers must follow a formal process, including giving the candidate a chance to respond.
Adverse Action
Adverse action happens when an employer decides not to hire someone based on information from a background check. Under the FCRA, the employer must provide a copy of the report and a summary of rights before making that decision final. This gives the candidate a fair opportunity to explain or correct the information.
Still have questions?
Get in touch with our team today for a personalized demo and discover how our tailored volume pricing and packages can drive results for your business!
How useful was this page?*
Note: your comments are anonymous. We use them to improve the website. Do not include any personal details.
Visit our FCRA Compliance Tool or leave a message here if you need a response.
From the blog Explore the GCheck Content Hub
DOT Physical Requirements for Drivers: 2026 Compliance Guide
9 Jan, 2026 • 17 min read
Healthcare Employee Background Check: What Employers Need to Know in 2026
9 Jan, 2026 • 19 min read
How Long Do Background Checks Take for Government Jobs? Timeline Expectations for 2026
6 Jan, 2026 • 20 min readThe information provided in this article is for general informational and educational purposes only and should not be construed as legal advice or a substitute for consultation with qualified legal counsel. While we strive to ensure accuracy, employment screening laws and regulations—including but not limited to the Fair Credit Reporting Act (FCRA), Equal Employment Opportunity Commission (EEOC) guidelines, state and local ban-the-box laws, industry-specific requirements, and other applicable federal, state, and local statutes—are subject to frequent changes, varying interpretations, and jurisdiction-specific applications that may affect their implementation in your organization. Employers and screening decision-makers are solely responsible for ensuring their background check policies, procedures, and practices comply with all applicable laws and regulations relevant to their specific industry, location, and circumstances. We strongly recommend consulting with qualified employment law attorneys and compliance professionals before making hiring, tenant screening, or other decisions based on background check information.

